Neonatal Quality Improvement 3
Session: Neonatal Quality Improvement 3
088 - Improving the rates of exclusive maternal milk at the time of NICU discharge, a quality improvement initiative
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 88.5479
Shruti Gupta, Yale School of Medicine, Westport, CT, United States; Katelyn Oconnor, Yale-New Haven Children's Hospital, Stamford, CT, United States; Zara N. Ilahi, Yale School of Medicine, Greenwich, CT, United States

Shruti Gupta, MB;BS (she/her/hers)
Medical Director of Neonatalogy, YNHH Greenwich Hospital
Yale School of Medicine
Westport, Connecticut, United States
Presenting Author(s)
Background: Maternal milk (MM) is the gold standard for infant nutrition and feeding. Aside from creating a bond between the mother and infant, there are numerous immunologic, nutritious, and neurodevelopmental benefits that breast milk has for preterm neonates.
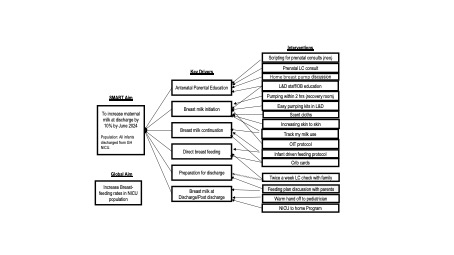
Objective: To increase the percentage of MM at discharge for newborns discharged from Greenwich Hospital (GH) NICU by 10% from 18% from March 2023 to June 2024.
Design/Methods: This is a one-step initiative quality improvement project assessing change before and after implementation of a global multi-disciplinary team initiative to increase MM rates at GH, a 15 bed-level III-B NICU. A simplified failure mode effect analysis was performed and key drivers were identified to analyze how we could improve exclusive MM at discharge. Areas for intervention were determined at 6 critical points: 1.) antenatal parental education 2.) breast milk initiation 3.) breast milk continuation 4.) direct breast feeding 5.) preparation for discharge and 6.) breast milk at NICU at discharge/post discharge. Interventions for each point are as follows: in the antenatal period, a lactation consultant (LC) met with the mother to start talking about MM. The NICU consult was scripted to highlight the importance of breastfeeding/MM. Home breast pumps were prescribed if mothers did not already have one. At birth, the NICU provider highlighted the importance of pumping, ordered a LC consult and the OB nurse ensured that pumping was initiated within 2 hours of delivery. Pumping kits were made accessible in L&D and scent clothes were used. To promote the continuation of MM/direct breastfeeding, skin to skin and oral immune therapy were encouraged, track my milk use was used (an online record on epic where mothers could log how much milk they pump), crib cards that showed what stage of feeding the baby was in were placed by the crib, and infant driven feeding principles were utilized. In preparation for discharge, a LC would check in with the mother twice weekly and feeding plans were discussed. At discharge, the pediatrician was notified about the feeding plan and babies were sent to the NICU to home program.
Results: Baseline data were collected from March 2023 to June 2024.By June 2024, on average 26% of infants were feeding exclusive MM at discharge.
Conclusion(s): The above interventions were successful in increasing exclusive MM at time of discharge by increasing the average rates by 8%. Further PDSA cycles will need to be done to ensure changes are sustainable and continue to be successful.
Key Driver Diagram
Run chart showing the percentage of MM at discharge
Exclusive MM at discharge graph.pdf


