Developmental and Behavioral Pediatrics 1: Parenting
Session: Developmental and Behavioral Pediatrics 1: Parenting
776 - Implementation and Feasibility of ‘Mothering from the Inside Out’ within Early Intervention Home Visiting: A Pilot Randomized Controlled Trial
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 776.5442
Elizabeth Peacock-Chambers, Baystate Children's Hospital, Springfield, MA, United States; Briana L. Jurkowski, Baystate Children's Hospital, Springfield, MA, United States; Emma R. Miller, Baystate Children's Hospital, Holyoke, MA, United States; Katie Gu, University of Massachusetts Medical School, Rohnert Park, CA, United States; Amanda Lowell, Yale School of Medicine, Springfield, MA, United States; Emily Feinberg, Brown University, Providence, RI, United States
- EP
Elizabeth Peacock-Chambers, MD, MS (she/her/hers)
Pediatrician
Baystate Children's Hospital
Springfield, Massachusetts, United States
Presenting Author(s)
Background: Parental substance use disorders (SUDs) are associated with long-term developmental and behavioral challenges for affected children. Greater access to evidence-based parenting support in early childhood is needed. Part C Early Intervention (EI) home visiting provides a potential setting where tailored evidence-based parenting supports for mothers in recovery may be disseminated.
Objective: To assess the 1) feasibility and 2) acceptability of Mothering from the Inside Out (MIO), and evidence-based parenting intervention designed specifically for mothers in recovery from SUDs, when delivered within EI.
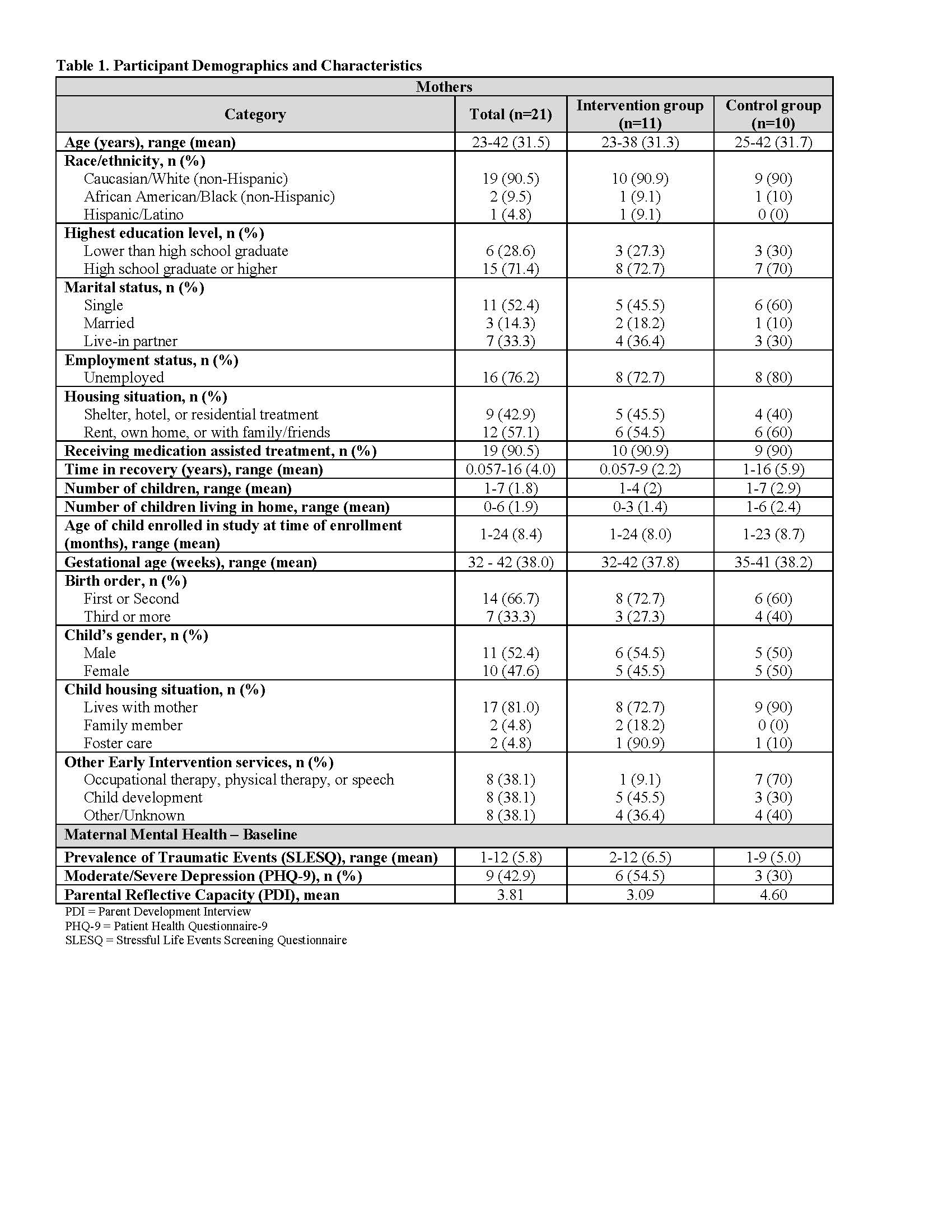
Design/Methods: We conducted a pilot randomized controlled trial took of MIO when delivered within the EI setting. To assess feasibility, we took an explanatory sequential mixed methods approach guided by the Consolidated Framework for Implementation Research (CFIR). Four mental health clinicians from 2 EI agencies in Massachusetts delivered MIO. Twenty-one mothers with SUDs and an index child between 0-2 years old enrolled in EI were randomly assigned to the intervention (n=11) or control (n=10) groups (Figure 1). Interpretation of feasibility measures (process and fidelity) were informed by qualitative analyses of exit interviews and field notes. Deductive codes from CFIR were used to categorize barriers and facilitators to implementation. Additional demographic characteristics, trauma history, depression, and parental reflective capacity were assessed at baseline using descriptive statistics.
Results: Eight control mothers completed all study assessments. Among the 11 MIO mothers, 3 completed all assessments, 4 completed full MIO treatment (≥8 sessions). At baseline, MIO mothers scored higher on depression and trauma and lower on reflective capacity scales (Table 1). Clinicians demonstrated maximal competency (3 out of 3) across all MIO sessions, while average frequency of MIO use was low (1.86 out of 3) on a standardized fidelity measure. We identified barriers and facilitators in the innovation, individual, and inner setting CFIR domains. The most significant barrier present across domains was inconsistency of delivery (Figure 2). Facilitators included benefit of MIO beyond the intended use, expanded scope of EI practice, and greater therapeutic alliance.
Conclusion(s): The delivery of MIO to mothers with SUDs within the EI setting was not feasible. The innovation itself as well as setting and individual characteristics contributed to a lack of consistent intervention delivery. Identified benefits of MIO may guide future adaptations for the EI setting or delivery via alternative venues.
Figure 1. Consort Diagram of Enrollment of Mother Participants
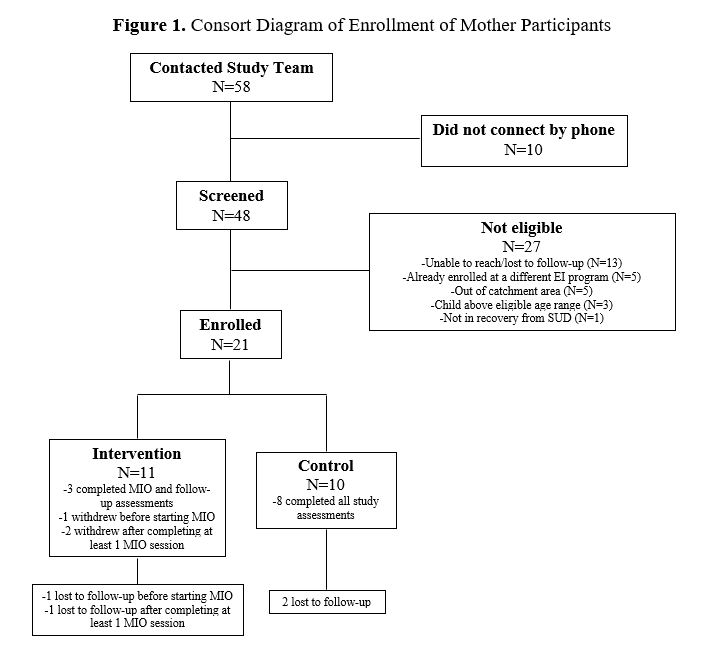
Figure 2. Thematic analysis of barriers and facilitators by Consolidated Framework for Implementation Research domains
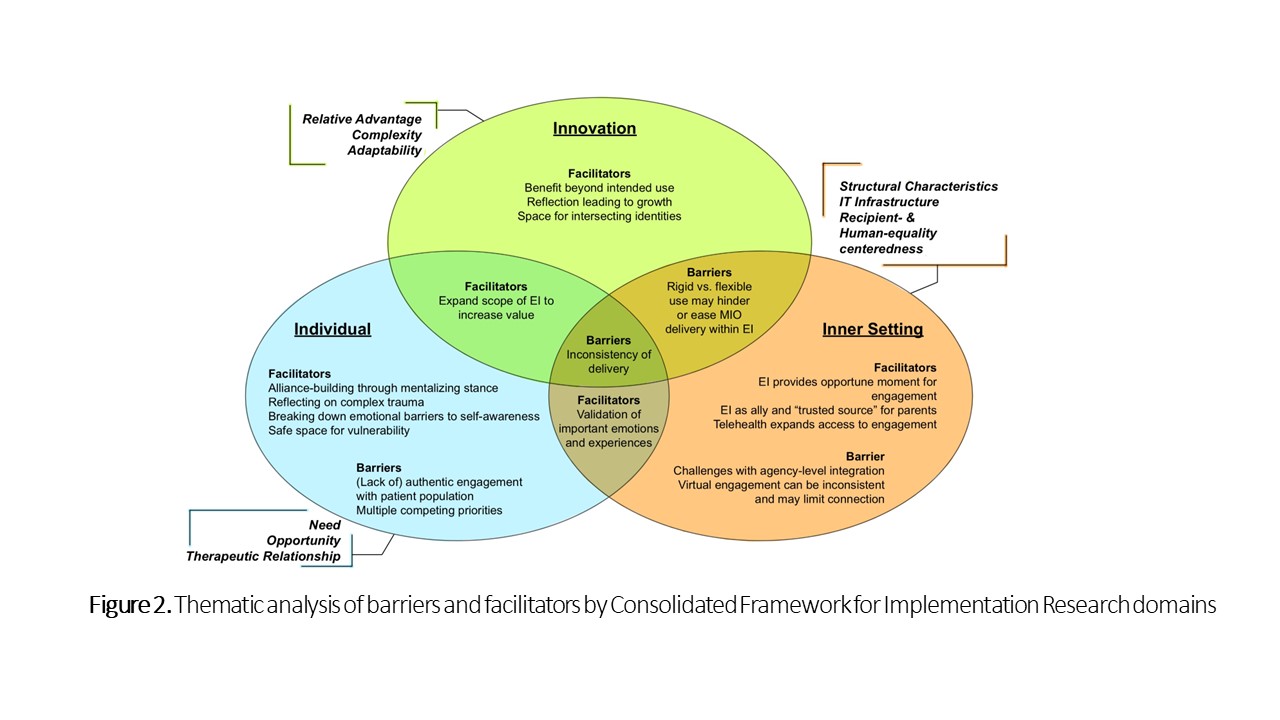
Table 1. Participant Demographics and Characteristics