Immunizations/Delivery 1
Session: Immunizations/Delivery 1
671 - Comparisons between Parent-Reported Vaccine Hesitancy and Vaccination Patterns, National Immunization Survey-Child 2018 and 2019
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 671.4299
Sophia R. Newcomer, University of Montana Center for Population Health Research, Missoula, MT, United States; Alexandria N. Albers, University of Montana, Missoula, MT, United States; Sarah Y. Michels, University of Montana, Missoula, MT, United States; Christina L. Clarke, Kaiser Permanente Institute for Health Research, Aurora, CO, United States; Jason Glanz, kaiser Permanente, Institute for Health Research, Aurora, CO, United States; Matthew Daley, Kaiser Permanente Colorado, Aurora, CO, United States

Sophia R. Newcomer, PhD, MPH (she/her/hers)
Associate Professor
University of Montana Center for Population Health Research
Missoula, Montana, United States
Presenting Author(s)
Background: Surveillance of vaccine hesitancy has focused on surveying parents about their vaccine attitudes and beliefs. However, prior work linking parents’ attitudes and beliefs to their vaccination behaviors has been limited.
Objective: To quantify the prevalence of parents’ vaccine concerns by child’s vaccination pattern during ages 0-24 months.
Design/Methods: We analyzed restricted-use data from the CDC’s National Immunization Survey-Child (NIS-Child) in 2018 and 2019. We quantified parents’ responses to 6 questions about vaccine hesitancy, overall and by vaccination pattern. To determine vaccination patterns, we analyzed provider-verified records for seven routine vaccines and assessed whether a child (1) received all vaccines on-time, (2) received all vaccines, but some were late, (3) started each of the seven vaccinations, but failed to complete ≥1 multidose series, (4) had some vaccines, but did not initiate ≥1 of the 7 series, or (5) were completely unvaccinated. Analyses accounted for the complex survey design, including weighting for nationally-representative estimates.
Results: Analyses included n=5,197 children. Overall, 22.9% (95% CI: 20.0%-25.7%) of parents stated they were somewhat or very hesitant about childhood shots. This prevalence was 14.9% among children vaccinated on-time, 23.4% among children who received all vaccines but some were late, 25.3% among children who failed to complete multidose series, 38.6% among children who had not started ≥1 series, and 65.6% among completely unvaccinated children. The percentage of parents who said that concerns about long-term side effects affected their decisions was highest among children who had not started ≥1 series (44.3%, 95% CI: 34.1%-54.5%) and completely unvaccinated children (67.9%, 95% CI: 49.4%-86.4%). Overall, 26.6% of parents whose child had not started ≥1 series and 43.5% of parents whose child was completely unvaccinated stated their child’s health care provider was not their most trusted source of vaccine information (Table 1).
Conclusion(s): Vaccine hesitancy was highest among parents whose children who were missing one or multiple vaccine series. Other key findings included that over 1 in 7 parents of children who received all vaccines on-time reported being vaccine-hesitant, and about one-third of parents of completely unvaccinated children reported not being hesitant. This latter finding suggests potential limitations of parents’ self-reported vaccine attitudes, missing vaccination records in the NIS, or non-attitudinal reasons for not receiving vaccines.
Table 1. Prevalence of parent-reported concerns about vaccinations, overall and by vaccination pattern, National Immunization Survey-Child 2018 and 2019
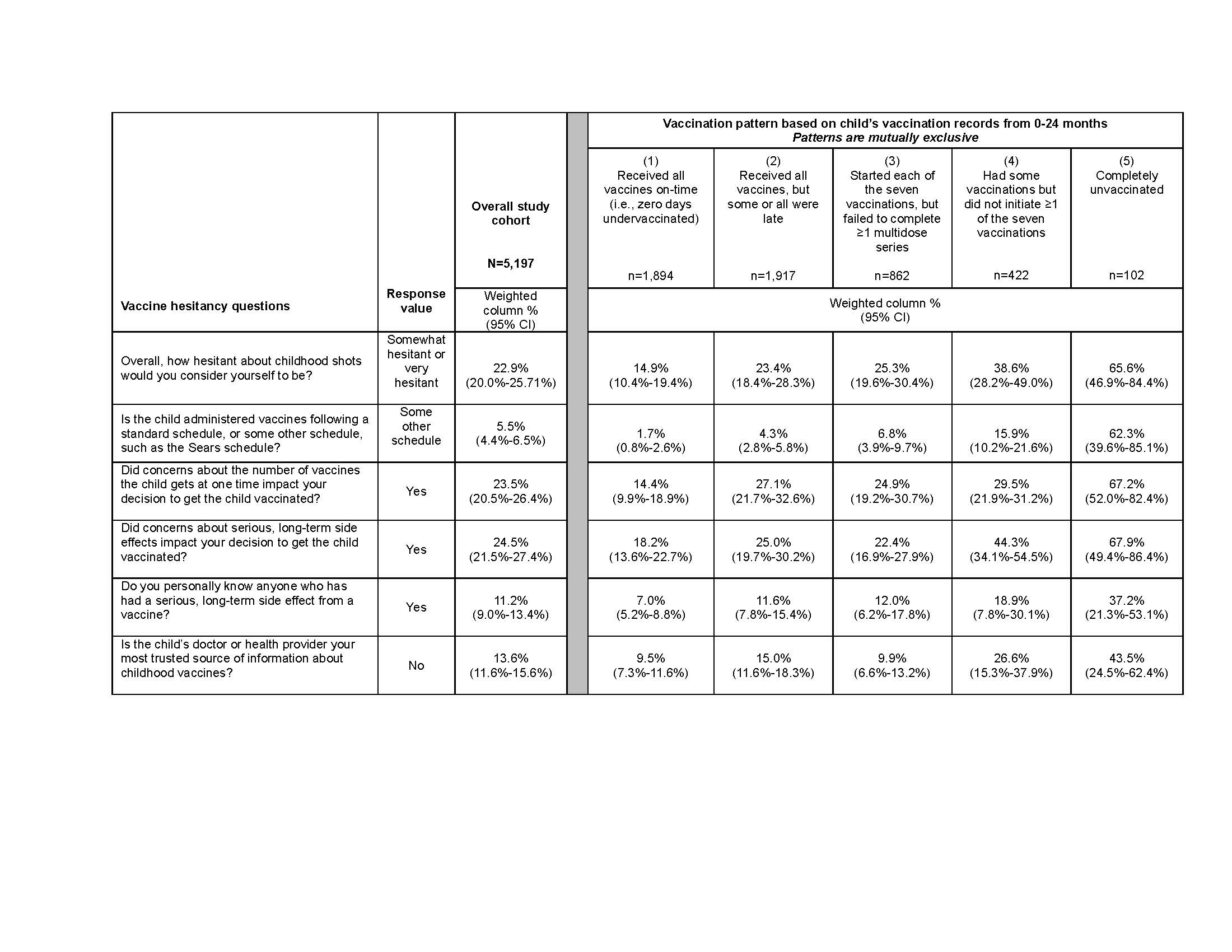 Table 1 caption: Analyses were conducted with data from children surveyed at ages 24-35 months whose parents answered at least one question in the vaccine hesitancy module. Vaccination patterns were assessed using the vaccinations included in the combined 7-vaccine series: hepatitis B, diphtheria-tetanus-and acellular pertussis, Haemophilus influenzae type b, pneumococcal conjugate, inactivated poliovirus, measles-mumps-rubella, and varicella vaccines. Responses of “don’t know” or “refused” were excluded from analyses for each question, resulting in denominators ranging from n=1842 to 1892 for analyses of hesitancy questions among children in Pattern 1, n=1868 to 1912 for Pattern 2, n=833 to 860 for Pattern 3, n=398 to 420 for Pattern 4, and n=71 to 100 for Pattern 5. We used a Rao-Scott chi-square to evaluate differences across vaccination patterns for each parental hesitancy questions; all p-values were < 0.001.
Table 1 caption: Analyses were conducted with data from children surveyed at ages 24-35 months whose parents answered at least one question in the vaccine hesitancy module. Vaccination patterns were assessed using the vaccinations included in the combined 7-vaccine series: hepatitis B, diphtheria-tetanus-and acellular pertussis, Haemophilus influenzae type b, pneumococcal conjugate, inactivated poliovirus, measles-mumps-rubella, and varicella vaccines. Responses of “don’t know” or “refused” were excluded from analyses for each question, resulting in denominators ranging from n=1842 to 1892 for analyses of hesitancy questions among children in Pattern 1, n=1868 to 1912 for Pattern 2, n=833 to 860 for Pattern 3, n=398 to 420 for Pattern 4, and n=71 to 100 for Pattern 5. We used a Rao-Scott chi-square to evaluate differences across vaccination patterns for each parental hesitancy questions; all p-values were < 0.001. 
