Neonatal General 4: Novel Technology and Therapies
Session: Neonatal General 4: Novel Technology and Therapies
798 - Fetal Heart Rate Tracing Characteristics Among Preterm Birth at 22.0-31.6 Weeks and Adverse Neonatal Outcomes
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 798.4859
Ha L. Tran, NemoursAlfred I. duPont Hospital for Children, PHILADELPHIA, PA, United States; Lauren London, Christiana Care Health Services, New castle, DE, United States; Fabrizio Zullo, Sapienza University of Rome, Rome, Lazio, Italy; Cassidy O’Sullivan, Christiana Care Health Services, Wilmington, DE, United States; Amanda J. Jones, Christiana Care Health System, Newark, DE, United States; Kelley Kovatis, ChristianaCare, Newark, DE, United States; Rachel L. Wiley, University of california san diego, San diego, CA, United States; Matthew K. Hoffman, CHRISTIANA CARE, Newark, DE, United States; Anthony Sciscione, Christiana Hospital, Newark, DE, United States; Suneet P. Chauhan, ChristianaCare Hospital, Newark, DE, United States

Ha L. Tran, MD (she/her/hers)
NICU Fellow
Nemours Alfred I. duPont Hospital for Children
PHILADELPHIA, Pennsylvania, United States
Presenting Author(s)
Background: Early identification of fetal distress in the intrapartum period is crucial to make informed decisions about labor management. As the standard of care in obstetrics, fetal heart rate tracing (FHRT) is used to assess the physiologic response to changes in fetal oxygenation. FHRT can prompt timely intervention to minimize the risk of intrauterine hypoxia. However, interpretation of FHRT remains variable and inconsistent, particularly among preterm births.
Objective: There is a paucity of evidence on the characteristics and significance of FHRT in the preterm population. This study aims to address this knowledge gap and explore the associated adverse neonatal outcomes.
Design/Methods: This study is a retrospective review of deliveries from January to December 2023 at a tertiary referral hospital. Criteria for inclusion were non-anomalous singleton deliveries at 22.0-31.6 weeks, where at least 10 minutes of FHRT were available. A physician—blinded to all outcomes—reviewed the FHRT (0-120 min prior to delivery) and outcome data was obtained from chart review. The primary outcome was long-term neonatal morbidity or mortality (LTNMM), defined as bronchopulmonary dysplasia or Grade 3-4 intraventricular hemorrhage. The secondary outcomes were a 5-min Apgar score of 4-6 and short-term neonatal morbidity or mortality (STNMM), defined as a 5-min Apgar score ≤ 3, metabolic acidosis on initial blood gas, or resuscitation involving intubation or chest compressions. Descriptive statistics with 95% confidence intervals (CI) were calculated with non-overlapping CI considered as significant.
Results: Among the 6,521 deliveries, 169 (2%) occurred at 22.0-31.6 weeks, of which 99 (58%) met the inclusion criteria. Intrapartum magnesium sulfate and corticosteroids were administered in 97% and 98% of deliveries, respectively. Moderate variability preceded delivery in 37.9% (95% CI 28.2-48.7%) of those with LTNMM; in 14.9% (95% CI 8.8-24.2%) of those with a 5-min Apgar score of 4-6; in 42.6% (95% CI 32.5-53.2%) of those with STNMM. Individuals with variable, late and prolonged decelerations had overlapping CI for all outcomes (Table 1). Of the 38 infants who met criteria for LTNMM, 20 (52.6%) also had STNMM while only 8 (21.1%) had Apgar of 4-6 at 5 min (Fig 1).
Conclusion(s): Among infants delivered at 22.0-31.6 weeks, the likelihood of 5-min Apgar score 4-6 and short- or long-term morbidity or mortality were similar irrespective of presence of moderate variability or decelerations. If confirmed, the reliance on moderate variability as a reassuring aspect to identify neonatal well-being at 22.0 to 31.6 weeks should be revisited.
Table 1
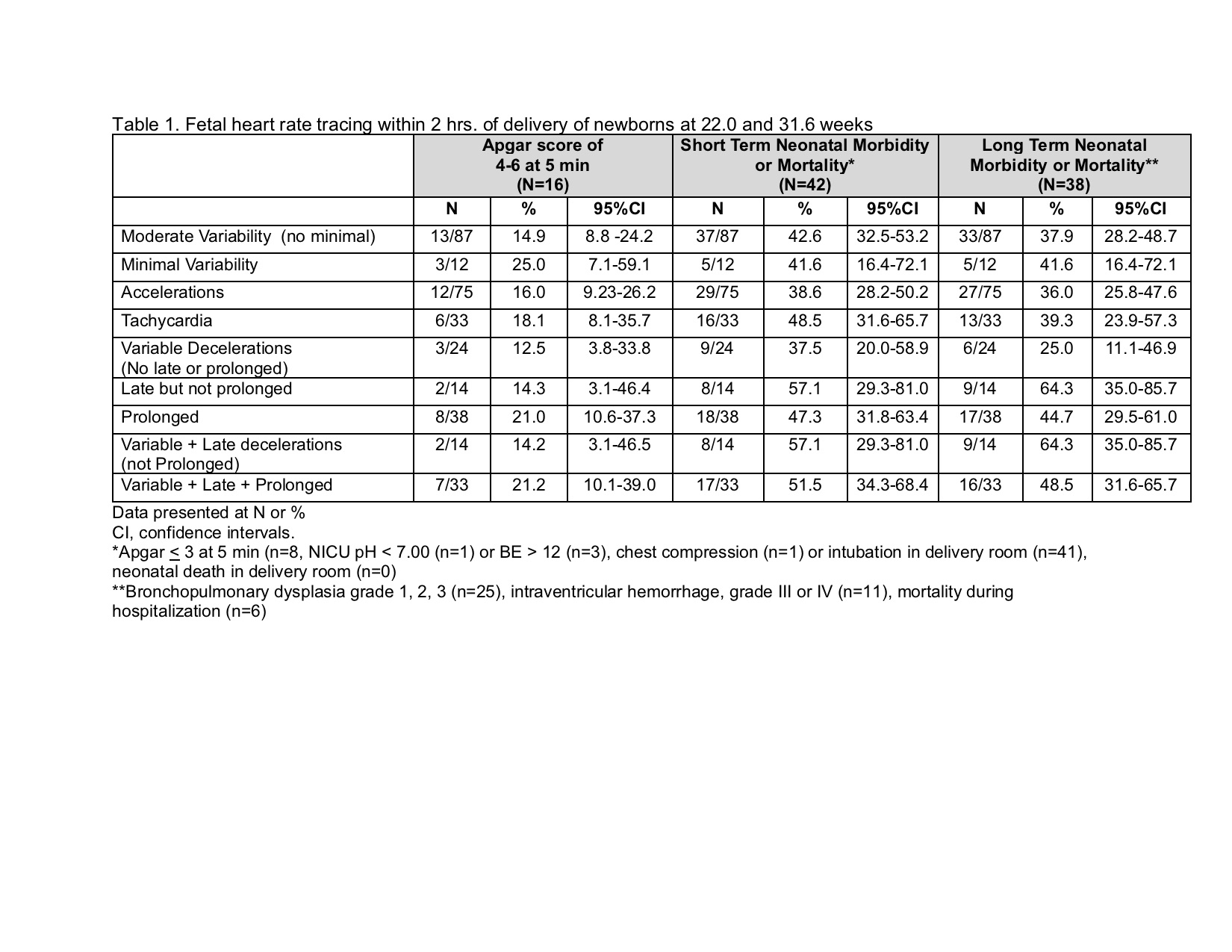 Fetal heart rate tracing within 2 hrs of delivery of newborns at 22.0 and 31.6 weeks
Fetal heart rate tracing within 2 hrs of delivery of newborns at 22.0 and 31.6 weeksFigure 1
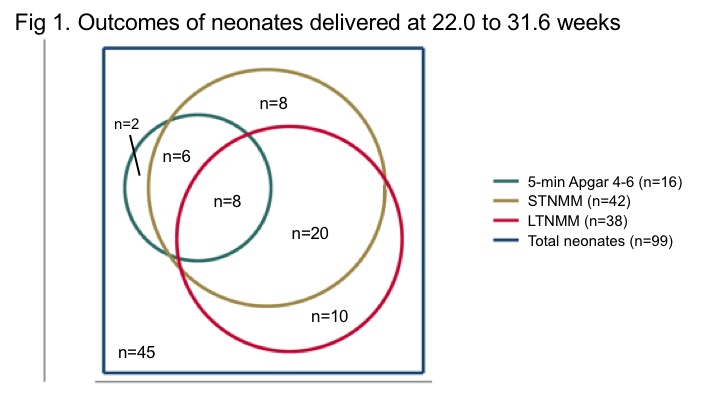 Outcomes of neonates delivered at 22.0 to 31.6 weeks
Outcomes of neonates delivered at 22.0 to 31.6 weeks
