Infectious Diseases 2: Bacterial infections
Session: Infectious Diseases 2: Bacterial infections
621 - Risk Factors for Surgical Site Infections in Infants following Congenital Heart Disease Surgery
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 621.6140
Ami J.. Patel, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; WooJin Shin, Columbia University Irving Medical Center, New York, NY, United States; Luis R. Alba, Columbia University Medical Center, New York, NY, United States; Maria Messina, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Cynthia Okerfelt, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Amelia O'Connell, Columbia University Vagelos College of Physicians and Surgeons, New york, NY, United States; Erin Driscoll, NewYork-Presbyterian Morgan Stanley Children's Hospital, Monroe, NJ, United States; Eva W. Cheung, Columbia Irving Medical Center, New York, NY, United States; Anita I. Sen, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Nimrod Goldshtrom, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Diana Vargas, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Angelica M. Vasquez, NewYork-Presbyterian Morgan Stanley Children's Hospital, Edgewater, NJ, United States; Ganga Krishnamurthy, Columbia University Medical Center, New York, NY, United States; Andrew B. Goldstone, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Emile Bacha, columbia university/Morgan Stanley Children's Hospital, New York NY 10032, NY, United States; Lisa Saiman, Columbia University, New York City, NY, United States

Ami J. Patel, MD (she/her/hers)
Clinical Fellow
Columbia University Vagelos College of Physicians and Surgeons
New York, New York, United States
Presenting Author(s)
Background: Neonates and infants requiring cardiothoracic (CT) surgery for CHD face increased morbidity and mortality if an associated SSI occurs. While studies identifying risk factors in adults undergoing CT surgery have been done, fewer data exist for neonates and infants who have unique risk factors due to their relative immunologic immaturity and complex cardiac lesions.
Objective: This study aims to identify potentially modifiable risk factors associated with SSIs in neonates and infants undergoing CHD surgery within the first year of life.
Design/Methods: This single center retrospective cohort study conducted from 2020-2023 assessed neonates and infants with CHD requiring CT surgery within their first year of life. SSIs were defined using Society of Thoracic Surgeons (STS) criteria. Demographic, pre-, intra-, and post-operative variables were collected using our institution’s STS database, infection prevention and control and quality databases, and chart review. Descriptive statistics including Chi-square tests, Fischer’s exact, and Student’s t-tests compared the characteristics of patients with and without SSIs.
Results: From 2020-2023, 60 (6.8%) of 879 patients developed an SSI of which 50%, 3%, and 47% were superficial, deep incisional, and mediastinitis, respectively. Age < 30 days at the time of surgery was associated with SSIs, while gestational age and birth weight were not. Cyanotic lesions, longer pre-operative hospitalization, and intubation prior to surgery were pre-operative factors associated with SSIs. Longer surgery and cardiopulmonary bypass times were intra-operative factors associated with SSIs. Open chest, temperature < 36 C° on ICU arrival, transfusion within 24 hours of surgery, and surgical re-exploration were post-operative factors associated with SSIs.
Conclusion(s): Infants undergoing CT surgery within their first 30 days of life and more medically and surgically complex infants with CHD may be at higher risk of SSIs. We found that hypothermia was associated with SSIs, suggesting this modifiable risk factor should be further assessed. The long duration of many surgeries suggests that intra-operative antibiotic redosing should also be assessed to decrease SSI risk. Social determinants of health, such as race and ethnicity, are associated with healthcare-associated infections in other populations but were not associated with SSIs in this population. Next, we plan to perform a multivariable analysis and analyze additional potentially modifiable risk factors, such as intra-operative redosing, hyperglycemia, and nutritional status.
Table 1: Demographic Characteristics of Neonates and Infants with and without SSIs
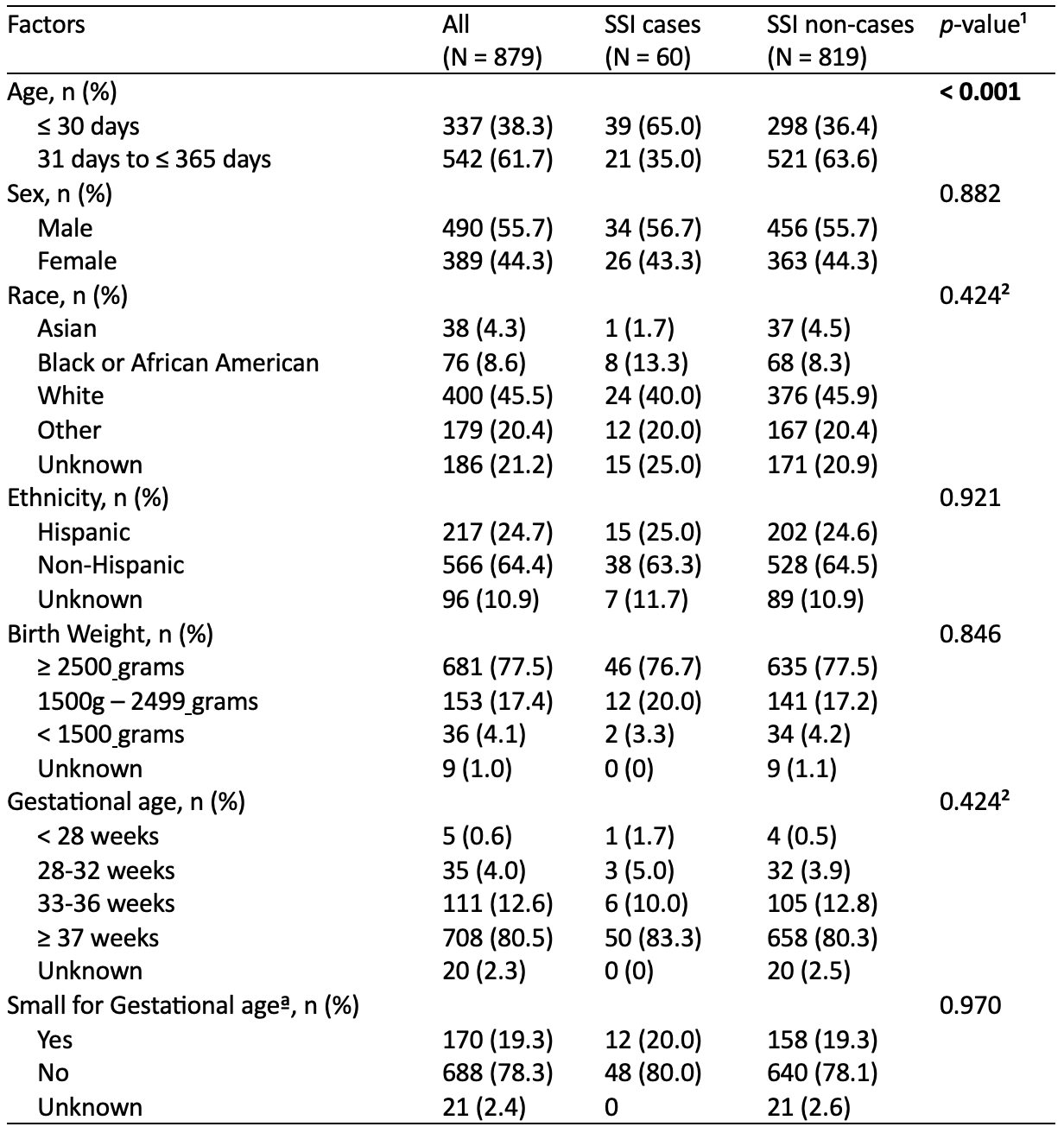 ¹p-value for χ² test statistic comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown values not included
¹p-value for χ² test statistic comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown values not included ²p-value for Fisher’s exact test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown values not included
ªNicole M. Talge, Lanay M. Mudd, Alla Sikorskii, Olga Basso; United States Birth Weight Reference Corrected for Implausible Gestational Age Estimates. Pediatrics May 2014; 133 (5): 844–853. 10.1542/peds.2013-3285
Table 2: Univariate analysis of pre-, intra-, and post-operative factors associated with SSIs
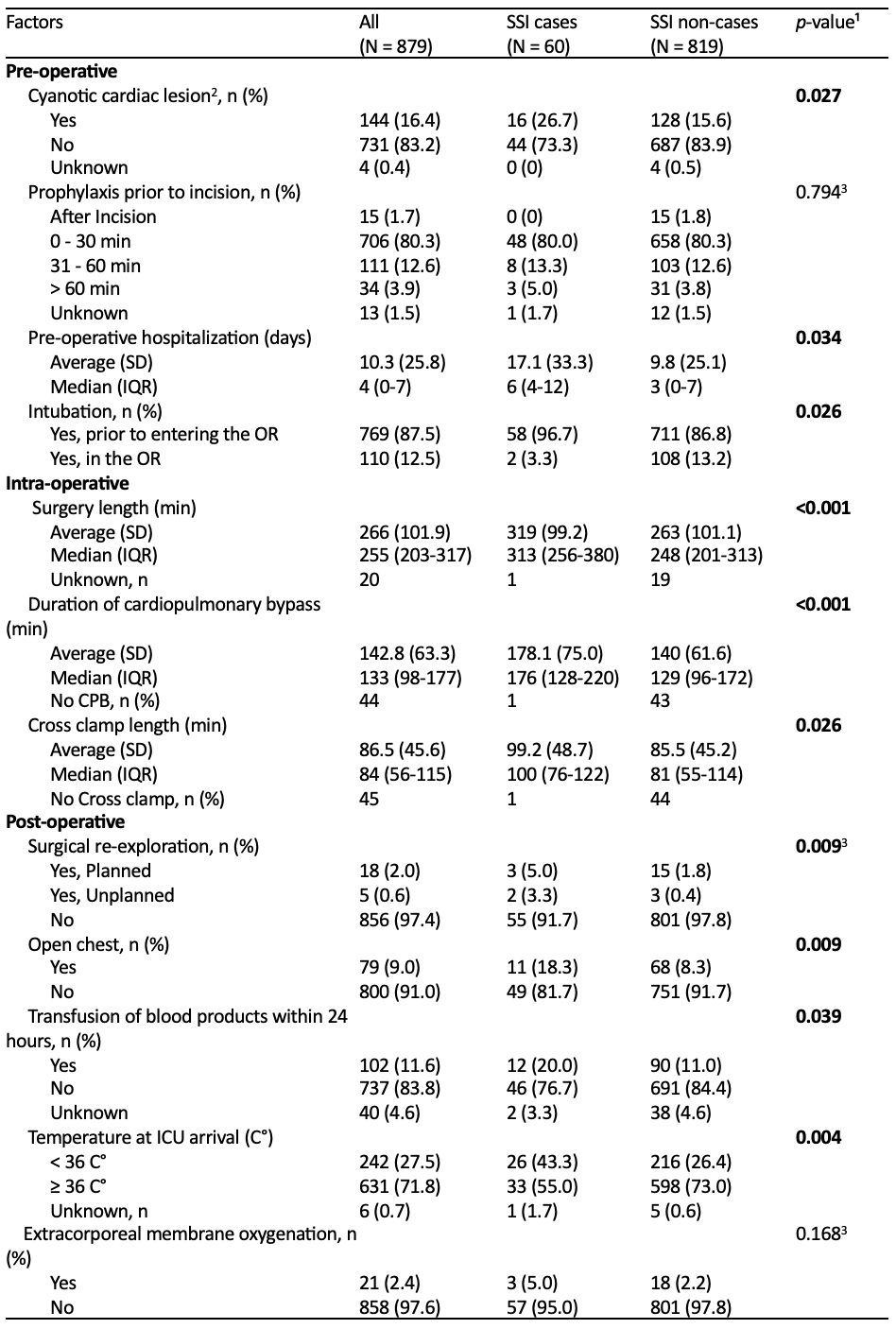 ¹p-value for χ² test statistic or 2-tailed t-test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown not included
¹p-value for χ² test statistic or 2-tailed t-test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown not included ²Yes = Pre-op O2 saturation ≤ 85, No = Pre-op O2 saturation > 85
³p-value for Fisher’s exact test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown not included
Table 1: Demographic Characteristics of Neonates and Infants with and without SSIs
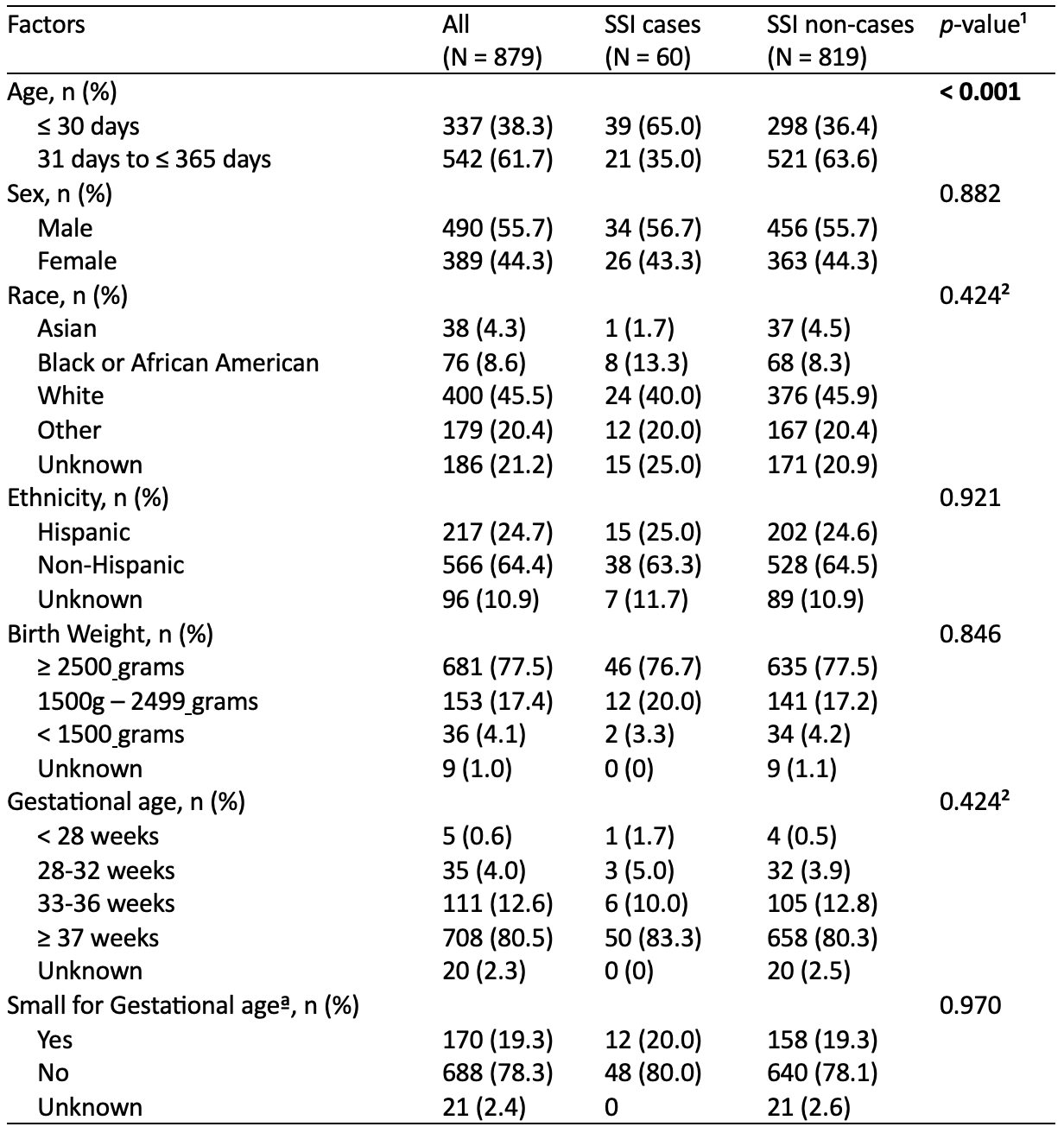 ¹p-value for χ² test statistic comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown values not included
¹p-value for χ² test statistic comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown values not included ²p-value for Fisher’s exact test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown values not included
ªNicole M. Talge, Lanay M. Mudd, Alla Sikorskii, Olga Basso; United States Birth Weight Reference Corrected for Implausible Gestational Age Estimates. Pediatrics May 2014; 133 (5): 844–853. 10.1542/peds.2013-3285
Table 2: Univariate analysis of pre-, intra-, and post-operative factors associated with SSIs
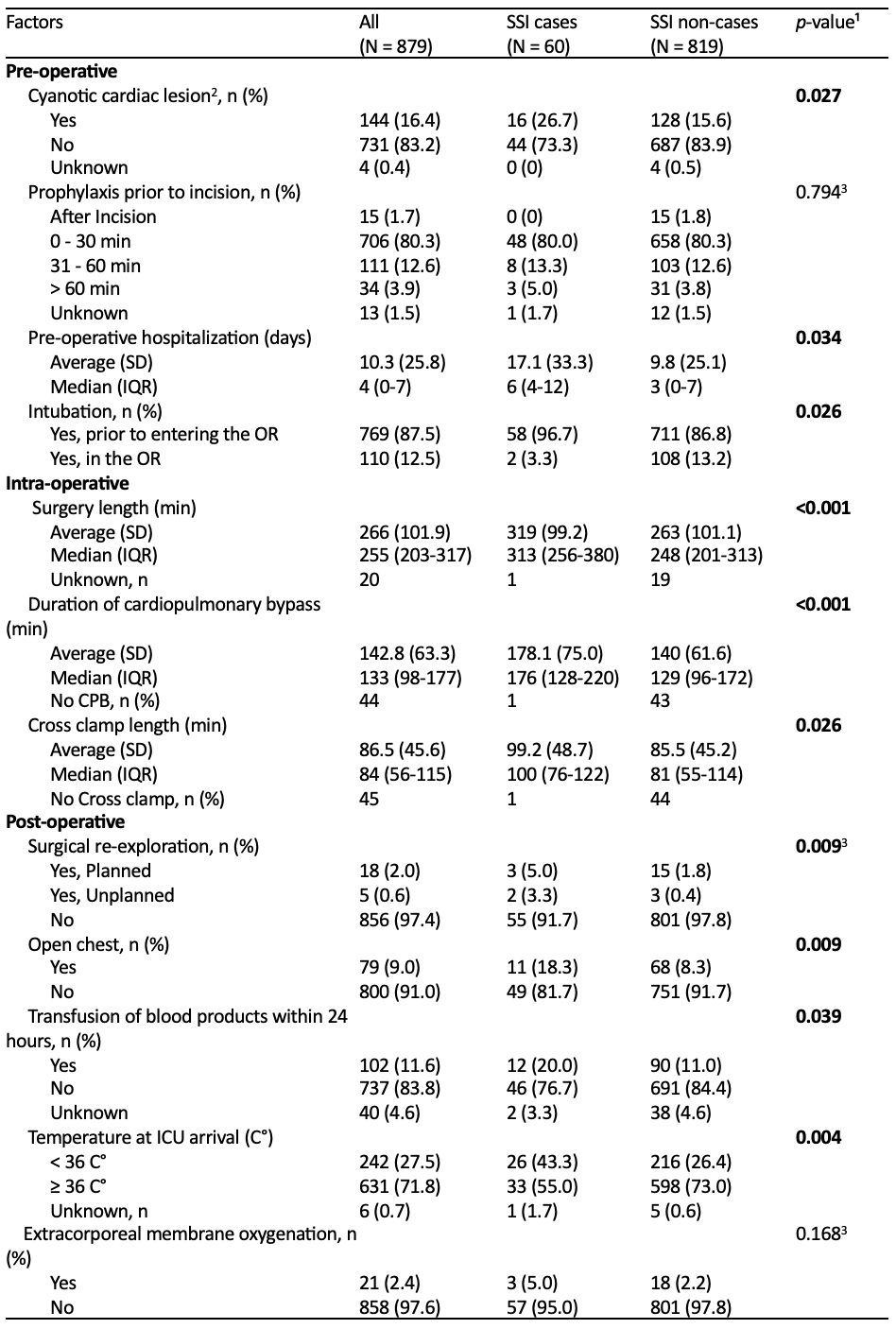 ¹p-value for χ² test statistic or 2-tailed t-test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown not included
¹p-value for χ² test statistic or 2-tailed t-test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown not included ²Yes = Pre-op O2 saturation ≤ 85, No = Pre-op O2 saturation > 85
³p-value for Fisher’s exact test comparing cases vs non-cases; p-value < 0.05 was used for significance, unknown not included

