Global Neonatal & Children's Health 1
Session: Global Neonatal & Children's Health 1
722 - Prediction of infant hospitalization and death using clinical features assessed by community health workers during routine postnatal household visits in Dhaka, Bangladesh
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 722.6154
Alastair Fung, The Hospital for Sick Children, Toronto, ON, Canada; Marimuthu Sappani, McMaster University, Hamilton, ON, Canada; Shaun Morris, Hospital for Sick Children and University of Toronto, Toronto, ON, Canada; Peter Gill, The Hospital for Sick Children, Toronto, ON, Canada; Chun-Yuan Chen, The Hospital for Sick Children, Toronto, ON, Canada; Diego G. Bassani, The Hospital for Sick Children, Toronto, ON, Canada; Davidson H. Hamer, Boston University School of Public Health, Cambridge, MA, United States; S M Abdul Gaffar, icddr,b, Dhaka, Dhaka, Bangladesh; Sultana Yeasmin, icddr,b, Dhaka, Dhaka, Bangladesh; Joseph Beyene, McMaster University, Hamilton, ON, Canada; Daniel Roth, The Hospital for Sick Children, Toronto, ON, Canada

Alastair Fung, MD, MPH (he/him/his)
Clinical Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Identification of potentially life-threatening illnesses among young infants ( < 2 months) by community health workers (CHWs) during routine home visits and subsequent referral to hospital are critical to reducing infant morbidity and mortality in low-resource settings.
Objective: To develop and internally validate a prediction model for hospitalization and/or death among young infants in Dhaka, Bangladesh using clinical features assessed by CHWs during routine home visits.
Design/Methods: This was a secondary analysis of 1939 generally healthy infants prospectively enrolled at birth at two public hospitals in Dhaka. CHWs assessed infants at up to 11 scheduled home visits from 3-60 days of age. The primary outcome was time to first hospitalization or death without hospitalization. Primary predictors included 45 clinical features (25 symptoms from caregiver history and 20 signs from physical exam) occurring on the day of a CHW visit or in the last 7 days. A prediction model was derived using time-varying Cox regression and internally validated using 5-fold cross-validation. Additional maternal and infant covariates (e.g., perinatal/delivery complication) were also included as predictors based on clinical judgment and if they improved model performance. Model discrimination was assessed using the C-statistic. We also evaluated the discrimination of the currently recommended World Health Organization (WHO) 8 danger signs to identify sick infants requiring referral during routine home visits.
Results: Of 1906 infants with at least one CHW home visit, 175 had an outcome event during the observation period (Table 1). The best-performing prediction model, consisting of any perinatal/delivery complication, application of a substance to the umbilical cord, systemic antibiotic administration, nasal congestion, rhinorrhea, cough, jaundice of the skin/eyes, and skin rash, obtained from caregiver history alone, had a C-statistic of 0.70 (95% CI 0.65-0.74) with a similar C-statistic on cross-validation (Table 2). WHO danger signs were infrequent ( < 0.1% of visits); a prediction model based on these signs had a C-statistic of 0.53 (0.52-0.55) (Table 3).
Conclusion(s): A prediction model for hospitalization and/or death using clinical information obtained from caregiver history alone during routine home visits from 3-60 days of age had acceptable discrimination and demonstrated higher discrimination than WHO danger signs. Since the predictors can be obtained from caregiver history alone, the model can be feasibly implemented via CHW telephone visits, without the need for in-person visits, but requires external validation.
Table 1. Baseline characteristics and additional covariates
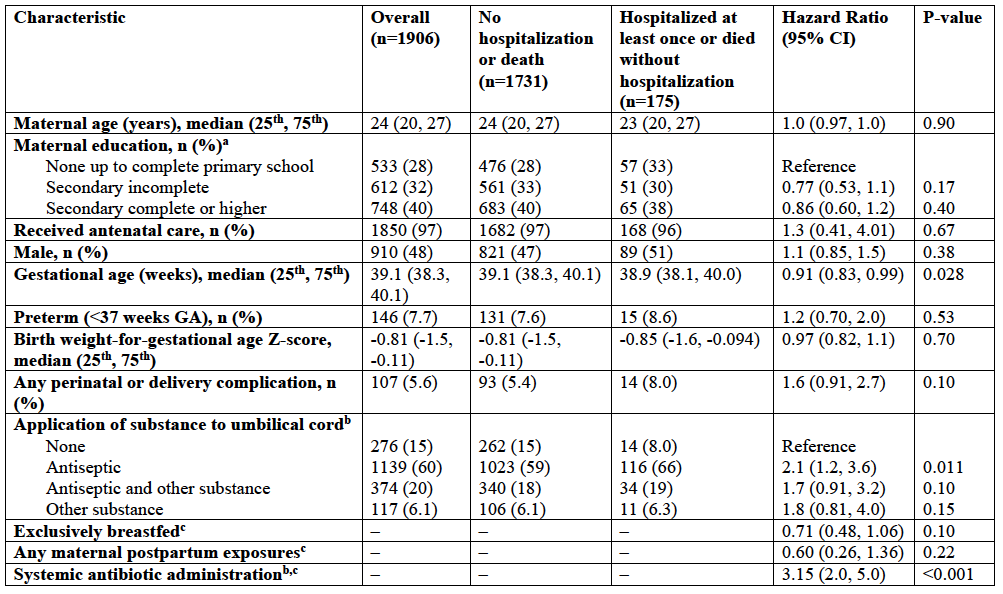 a Denominator is the number of mothers (n=1893).
a Denominator is the number of mothers (n=1893).b Since the direction of effect is in the direction of increasing risk of hospitalization and/or death, the application of a substance to the umbilical cord and administration of a systemic antibiotic were assumed to have been done in response to a clinical concern (e.g., signs of inflammation in the case of application of a substance to the umbilical cord), but this could not be confirmed based on the available data.
c Observation window: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
Table 2. Predictive accuracy of prediction model for hospitalization and/or death among young infants assessed by community health workers during routine home visits from 3-60 days of age
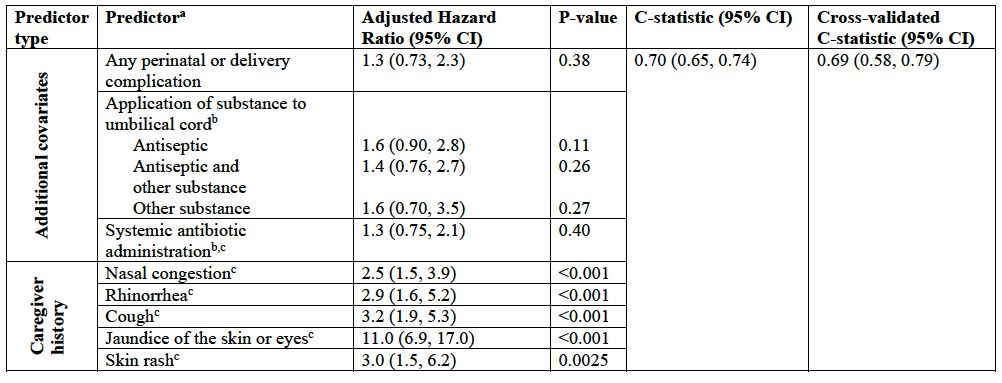 a Predictors from caregiver history selected using backward selection based on threshold p-value of <0.2. Additional covariates included as predictors based on clinical judgment and if they improved model performance (C-statistic).
a Predictors from caregiver history selected using backward selection based on threshold p-value of <0.2. Additional covariates included as predictors based on clinical judgment and if they improved model performance (C-statistic).b Since the direction of effect is in the direction of increasing risk of hospitalization and/or death, the application of a substance to the umbilical cord and administration of a systemic antibiotic were assumed to have been done in response to a clinical concern (e.g., signs of inflammation in the case of application of a substance to the umbilical cord), but this could not be confirmed based on the available data.
c Observation window: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
Table 3. Predictive accuracy of the World Health Organization (WHO) 8 danger signs for hospitalization and/or death among young infants assessed by community health workers during routine home visits from 3-60 days of age
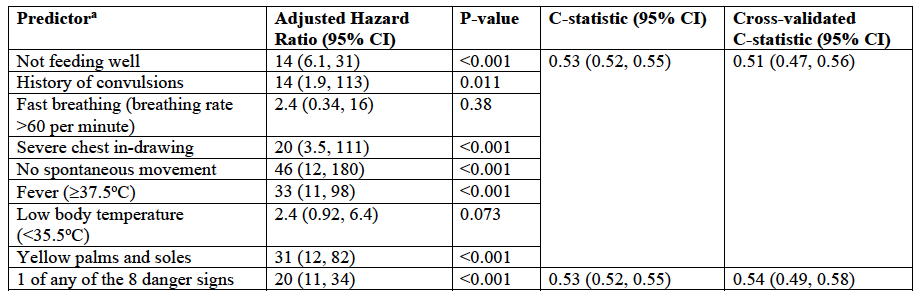 a Observation window for predictors: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
a Observation window for predictors: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).Table 1. Baseline characteristics and additional covariates
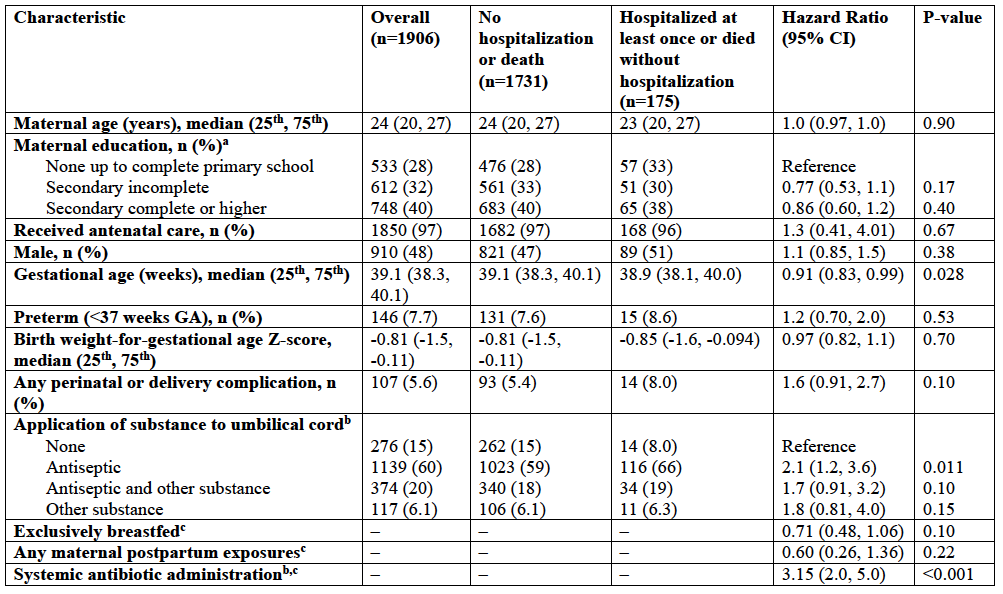 a Denominator is the number of mothers (n=1893).
a Denominator is the number of mothers (n=1893).b Since the direction of effect is in the direction of increasing risk of hospitalization and/or death, the application of a substance to the umbilical cord and administration of a systemic antibiotic were assumed to have been done in response to a clinical concern (e.g., signs of inflammation in the case of application of a substance to the umbilical cord), but this could not be confirmed based on the available data.
c Observation window: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
Table 2. Predictive accuracy of prediction model for hospitalization and/or death among young infants assessed by community health workers during routine home visits from 3-60 days of age
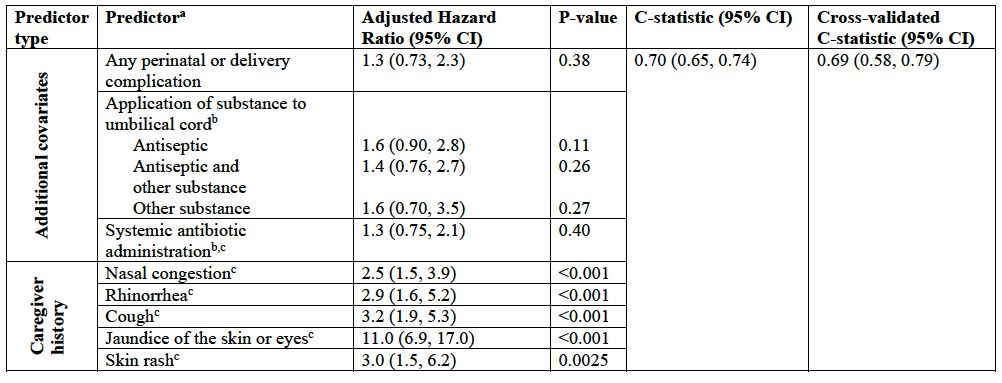 a Predictors from caregiver history selected using backward selection based on threshold p-value of <0.2. Additional covariates included as predictors based on clinical judgment and if they improved model performance (C-statistic).
a Predictors from caregiver history selected using backward selection based on threshold p-value of <0.2. Additional covariates included as predictors based on clinical judgment and if they improved model performance (C-statistic).b Since the direction of effect is in the direction of increasing risk of hospitalization and/or death, the application of a substance to the umbilical cord and administration of a systemic antibiotic were assumed to have been done in response to a clinical concern (e.g., signs of inflammation in the case of application of a substance to the umbilical cord), but this could not be confirmed based on the available data.
c Observation window: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
Table 3. Predictive accuracy of the World Health Organization (WHO) 8 danger signs for hospitalization and/or death among young infants assessed by community health workers during routine home visits from 3-60 days of age
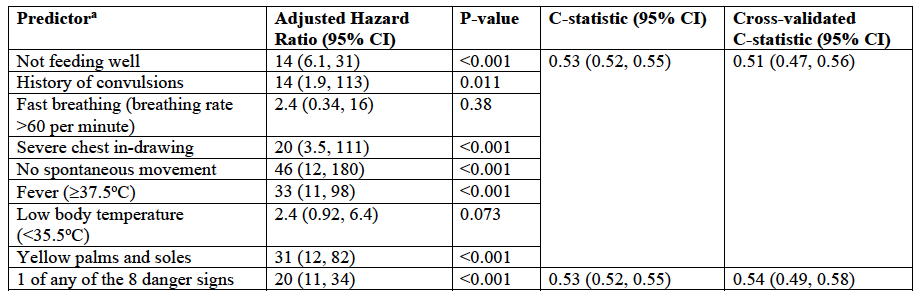 a Observation window for predictors: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
a Observation window for predictors: In the last 7 days including the day of the home visit or since the last home visit (whichever is most recent).
