Developmental Biology/Cardiac & Pulmonary Development
Session: Developmental Biology/Cardiac & Pulmonary Development
179 - Maternal-Fetal Interactions in a Novel In-Vivo Model of Maternal ARDS
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 179.5771
Michelle J. Lim, University of California, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Xiaohan Li, University of California Davis, Davis, CA, United States; Rebecca Valdez, University of California Davis, Davis, CA, United States; Amy Lesneski, University of California, Davis, School of Medicine, Davis, CA, United States; Jocelyn Livezey, University of California, Davis, School of Medicine, Encinitas, CA, United States; Victoria Hammitt, University of California, Davis, School of Medicine, Sacramento, CA, United States; Erin Riley, University of California, Davis, School of Medicine, Redding, CA, United States; Kent E. Pinkerton, University of California, Davis, School of Medicine, Davis, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States
- ML
Michelle J. Lim, MD (she/her/hers)
Assistant Professor
University of California
Sacramento, California, United States
Presenting Author(s)
Background: Pregnancy is a common risk factor for severe pneumonia and acute respiratory distress syndrome (ARDS). There is a limited understanding of the complex relationship of maternal-fetal interactions with acute hypoxia and systemic inflammation in ARDS during pregnancy, limiting a goal-directed care approach and at the consequence of poor outcomes. The impact of maternal ARDS on fetal oxygenation and hemodynamics is unknown.
Objective: To understand the effect of maternal hypoxia on fetal oxygenation and hemodynamics in a preterm ovine model of maternal ARDS.
Design/Methods: Lung injury was induced in pregnant ewes at preterm gestation (132-135 d, term ~ 147d) using CASP (combined acid plus small gastric particles, 1ml/kg) following surgical instrumentation of maternal ewe and fetus in-utero (Figure 1). Fetal lambs were placed back in the uterus, and blood gases and hemodynamics were monitored for 4 hours after injury. Data analysis was performed using non-parametric statistics.
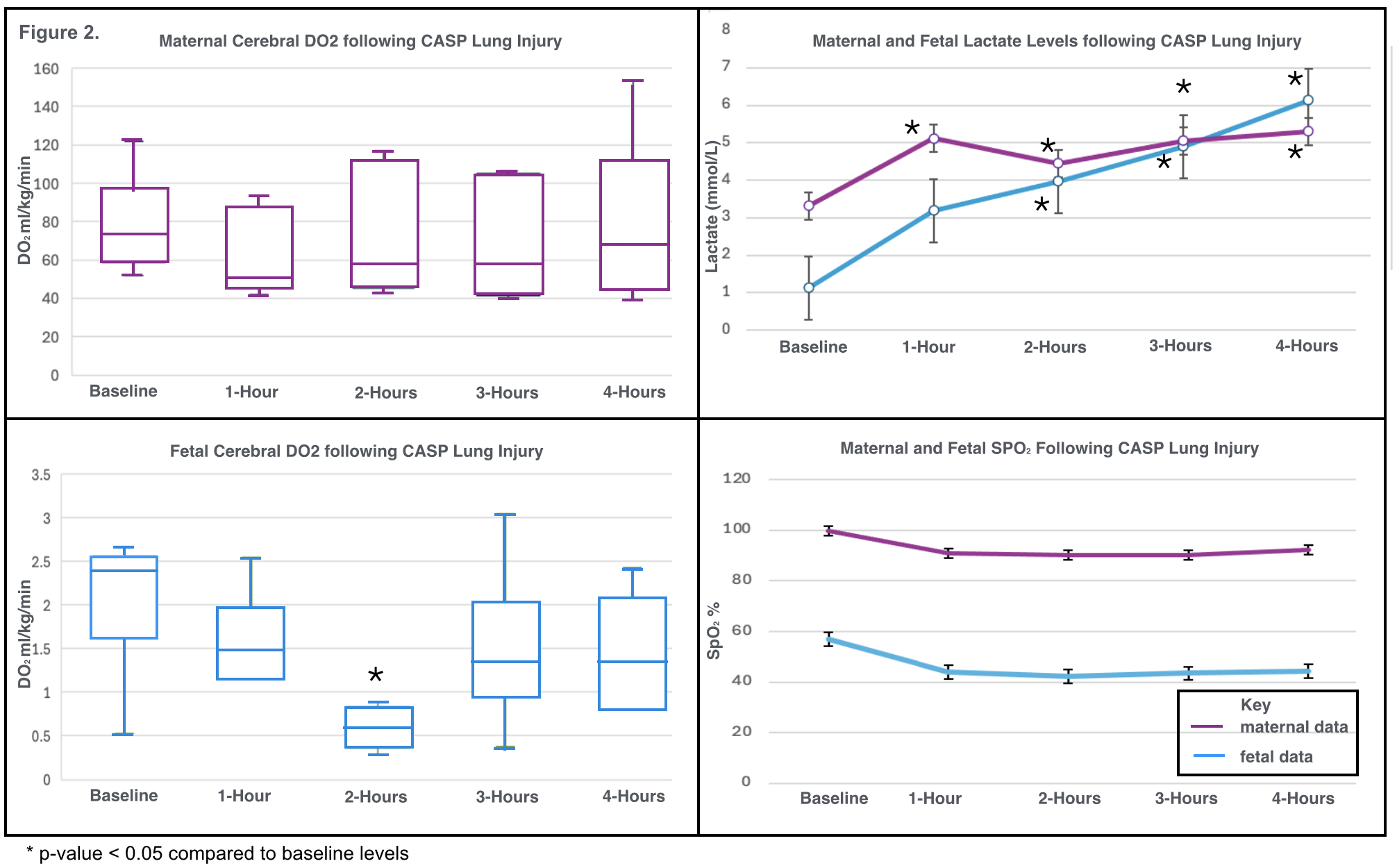
Results: Seven pregnant ewes were included in the analysis. Median PaO2/FiO2 ratios were 370 [IQR 264-445] prior to CASP administration and decreased to 119 [ IQR 82-164] within 30 min (p=0.01) and maintained at these levels throughout the study (Figure 2). Although no significant change in maternal cerebral oxygenation was observed, a ~30% reduction in fetal brain oxygen delivery was observed at study end, with a critically significant nadir at 2 hours (p=0.007) (Figure 3). Maternal and fetal lactate significantly increased from baseline following CASP injury. One fetal death in-utero occurred, and all other lambs survived to study-end. Fetal hemodynamics in-utero were within normal limits for all surviving lambs, although fetal heart rate was higher at study-end (mean 144 bpm vs 125, 95% CI 132-156, p=0.04). Mean fetal pH and SpO2 at 5-min and 60-min post-birth were 7.1 (sd 0.1) and 63% (sd 32) and 7.3 (sd 1.2) and 94% (sd 8.1). Histopathology of maternal lungs demonstrated moderate-severe inflammation, with influx of alveolar neutrophils and capillary barrier disruption.
Conclusion(s): In a novel preterm model of maternal ARDS, maternal cerebral oxygen delivery is preserved following hyperoxic ventilation at the expense of compromised fetal cerebral oxygen delivery, resulting in 14% fetal death rate and low fetal pH and hypoxia at birth. Pregnant persons with ARDS are at increased risk of poor perinatal outcomes, despite reassuring parameters of maternal oxygenation and fetal hemodynamics and must be closely monitored. Clinical management of optimal oxygenation and ventilation parameters in ARDS must be further assessed in pregnancy.
Figure 1. Preterm Ovine Model of Maternal ARDS
.png)
Figure 2. Maternal Hypoxemia following CASP Injury and Histopathology of ARDS
.png)
Figure 3. Maternal-Fetal Interactions Following CASP Injury