Neonatal General 2: Neurology
Session: Neonatal General 2: Neurology
328 - Prevalence of Delirium and Patient Characteristics in a Level IV NICU
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 328.6415
Divya Rana, UTHSC, Memphis, TN, United States; Kathryn E. Martin, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States; Mark F. Weems, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States
- DR
Divya Rana, MD (she/her/hers)
Associate Professor
UTHSC
University of Tennessee Health Science Center
Memphis, Tennessee, United States
Presenting Author(s)
Background: Delirium is an under-researched condition in neonatal intensive care units (NICUs), despite its recognized impact in pediatric intensive care units (PICUs). The Cornell Assessment for Pediatric Delirium (CAPD) is a reliable tool for delirium diagnosis in critical care settings. This study aims to determine the prevalence of delirium in a Level IV NICU and examine basic patient characteristics associated with this condition.
Objective: Prevalence of delirium as defined by Cornell Assessment for Pediatric Delirium (CAPD) at a Level IV NICU
Design/Methods: This retrospective cohort study included infants ≥40 weeks post-menstrual age (PMA) admitted to a Level IV NICU, who had at least one documented CAPD score between April 1, 2023, and March 31, 2024. A CAPD score of ≥9 indicated delirium. CAPD score is administered as standard of care in NICU. Patient characteristics such as gestational age at birth, birth weight, length of hospital stay, and mortality rates were analyzed in relation to delirium status.
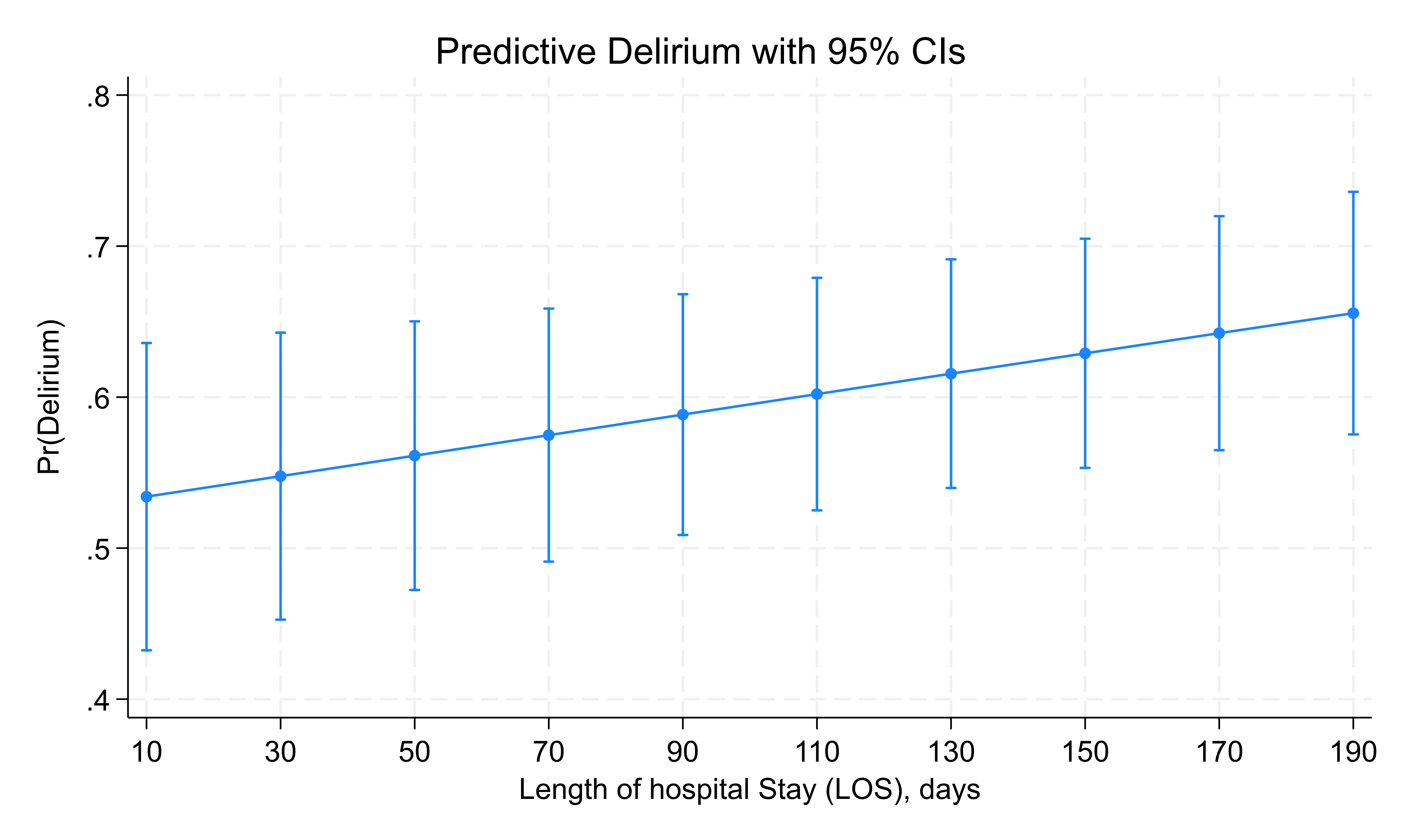
Results: Among 153 infants, 99 (65%) met the diagnostic criteria for delirium. Infants with delirium had a significantly lower median gestational age at birth (30 weeks) compared to those without delirium (37 weeks, p < 0.01). The median birthweight of infants with delirium was also lower (1120 g) compared to non-delirious infants (2360 g, p < 0.01). Infants on mechanical ventilation at the time of high CAPD score were more likely to experience delirium compared to those not on ventilation, p < 0.001, table 1. Regression analysis showed that each additional week of gestational age, the odds of experiencing delirium decrease by approximately 11%, OR 0.894 (95% CI: 0.841 to 0.951, p < 0.001). Delirium was associated with longer hospital stays, with a median stay of 119 days versus 41 days for infants without delirium (p < 0.01), the odds of experiencing delirium increase by approximately 0.4% with each additional day of length of stay, with an odds ratio of 1.006 (95% CI: 1.003 to 1.009, p < 0.001), figure 1. Moreover, 20% of infants with delirium died prior to discharge compared to only 5% of non-delirious infants (p < 0.01).
Conclusion(s): Delirium is prevalent in NICU patients, especially in infants with lower birthweight, gestational age and requiring mechanical ventilation. The condition is also linked to significantly longer hospital stays and increased mortality. These findings underscore the need for heightened awareness and routine screening for delirium in this high-risk population with risk mitigation strategies.
Table 1. Clinical Characteristics of Infants by Delirium
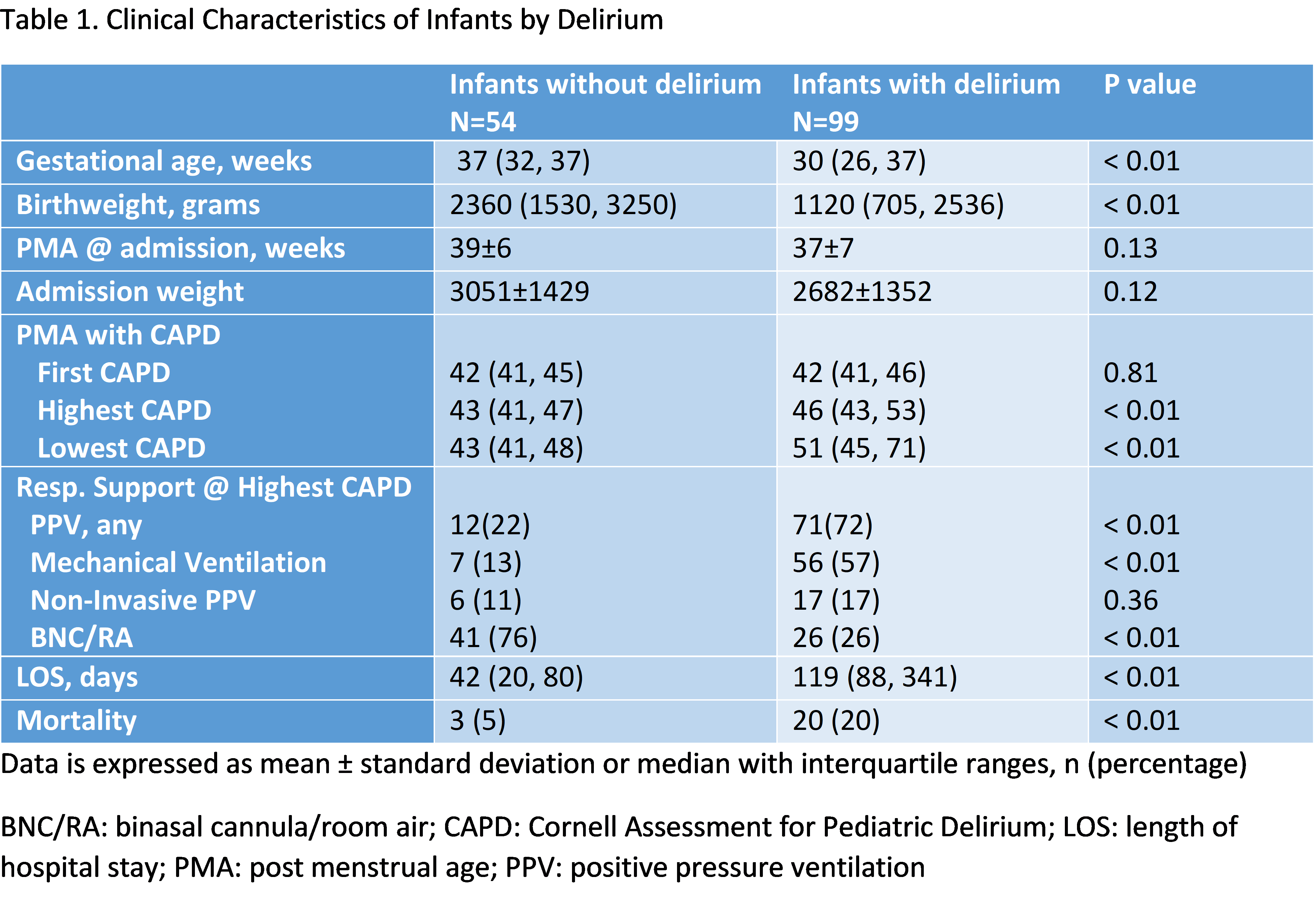
Figure 1: Delirium by Length of Hospital Stay