Neonatal/Infant Resuscitation 1
Session: Neonatal/Infant Resuscitation 1
283 - Optimizing oxygen delivery in neonatal resuscitation by using self-inflating bags without air-oxygen blenders
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 283.5938
Tzu-Ching Sung, I-Shou University, Kaohsiung, Kaohsiung, Taiwan (Republic of China); Chyi-her Lin, E-Da Hosp., Tainan, Tainan, Taiwan (Republic of China); Yun-Ju Chen, NCKU hospital, Tainan, Tainan, Taiwan (Republic of China); Yuh Jyh Lin, National Cheng Kung University Hospital, Tainan, Tainan, Taiwan (Republic of China); Hsiang-Chin Hsu, National Cheng Kung University College of Medicine, Tainan, Tainan, Taiwan (Republic of China)
- CL
Chyi-Her Lin, MD (he/him/his)
Consultant Pediatrician
E-Da Hosp.
Tainan, Tainan, Taiwan (Republic of China)
Presenting Author(s)
Background: Newborns, especially preterm infants, are susceptible to oxygen-induced toxicity. Current guidelines recommend initiating resuscitation with a fraction of inspired oxygen (FiO₂) between 0.21 and 0.30 for infants born less than 35 weeks gestation. However, in settings without an air-O₂ blender, titrating FiO₂ poses a challenge.
Objective: This in-vitro study investigated the effects of peak inspiratory pressure (PIP), ventilation rates (VRs), and oxygen flow rates (FRs) on FiO₂ when ventilating with a self-inflating resuscitation bag (SIRB).
Design/Methods: We used two types of SIRBs: a bag with a 280 mL capacity (40 cm H₂O pressure-relief valve), and a 62 mL bag (25 cm H₂O pressure-relief valve). Both SIRBs were supplied with 100% oxygen and connected to a pressure gauge, oxygen analyzer, and an artificial lung. We tested combinations of FRs (0.5, 1, 2, 5, or 10 L/min), PIPs (20–29, 30–39, or ≥40 cm H₂O), and VRs (40, 50, or 60/min), sequentially. We performed each combination setting thrice and measured FiO₂ every 30 sec over 150 sec. All data points were systematically collected for stepwise generalized linear model analysis.
Results: A total of 450 settings were recorded. FiO₂ levels increased and reached a plateau in 60-90 sec across all settings. SIRBs with 280 mL and 62 ml capacity produced maximal FiO₂ up to 0.8 and 1.0. FiO₂ were positively correlated with FRs and stepwise increasing PIP from 20-30 cm H₂O to >40 cm H₂O reduced FiO₂. Increasing VR from 40/min to 60/min did not increase FiO₂ unless oxygen FRs were ≥5 L/min. FiO₂ 0.30 was only achievable using the 280 mL SIRB with FR of 0.5 L/min and PIP above 40 cm H₂O. FR was the main factor affecting the model (R2 = 0.4916), and adding SIRB further increased the model's predictive power (R2 = 0.8855). Including PIP and duration of oxygen delivery, plus VR and duration of bagging further enhanced the predictive model (R2 = 0.9578).
Conclusion(s): FR and the capacity of the SIRB are major determinants of FiO₂ level. Increasing FR to maintain FiO₂ is required if PIP or VR is elevated. Studies to validate these results in clinical applications are warranted.
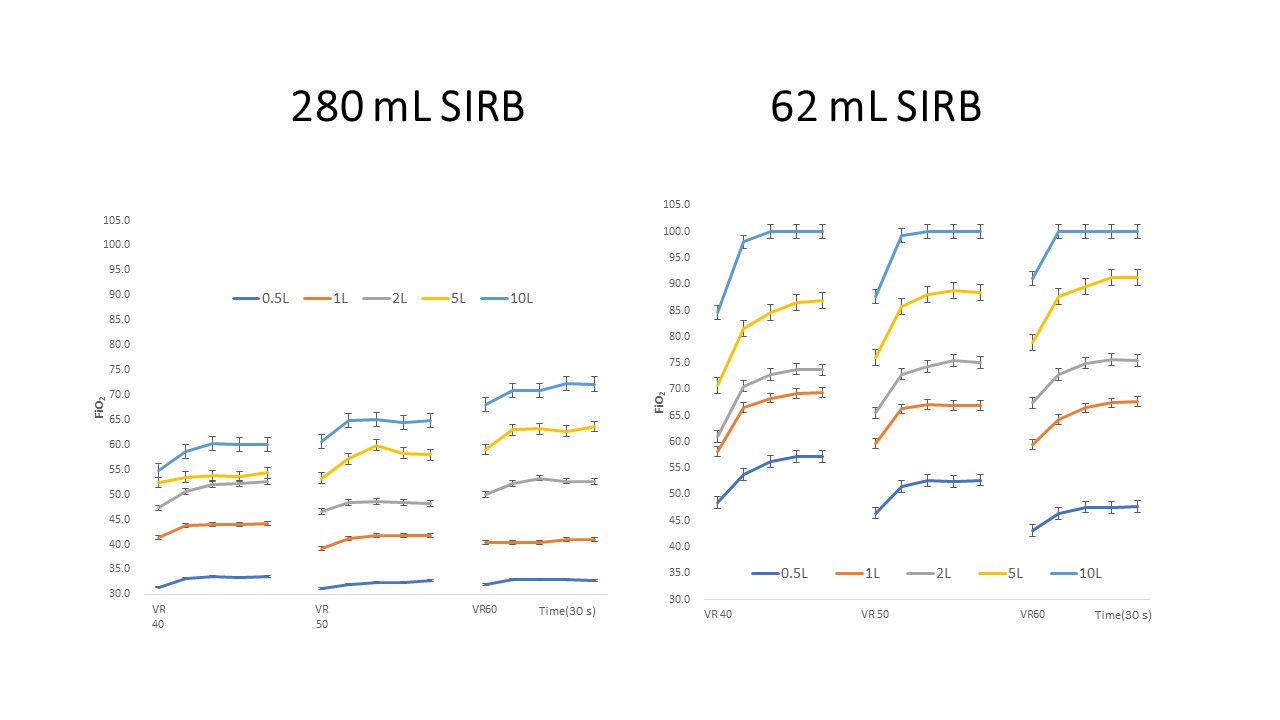
Figure 1
.jpg) Interaction of panel plots among the SIRB of 280 mL or 62 mL capacity, ventilation rates (VR), and oxygen flow rates (L/min) at 20-29 cm H₂O peak inspiratory pressure over time (150 sec).
Interaction of panel plots among the SIRB of 280 mL or 62 mL capacity, ventilation rates (VR), and oxygen flow rates (L/min) at 20-29 cm H₂O peak inspiratory pressure over time (150 sec).Figure 2
 Interaction of panel plots among the SIRB of 280 mL or 62 mL capacity, ventilation rates (VR), and oxygen flow rates (L/min) at 30-39 cm H₂O peak inspiratory pressure over time (150 sec).
Interaction of panel plots among the SIRB of 280 mL or 62 mL capacity, ventilation rates (VR), and oxygen flow rates (L/min) at 30-39 cm H₂O peak inspiratory pressure over time (150 sec).Figure 3
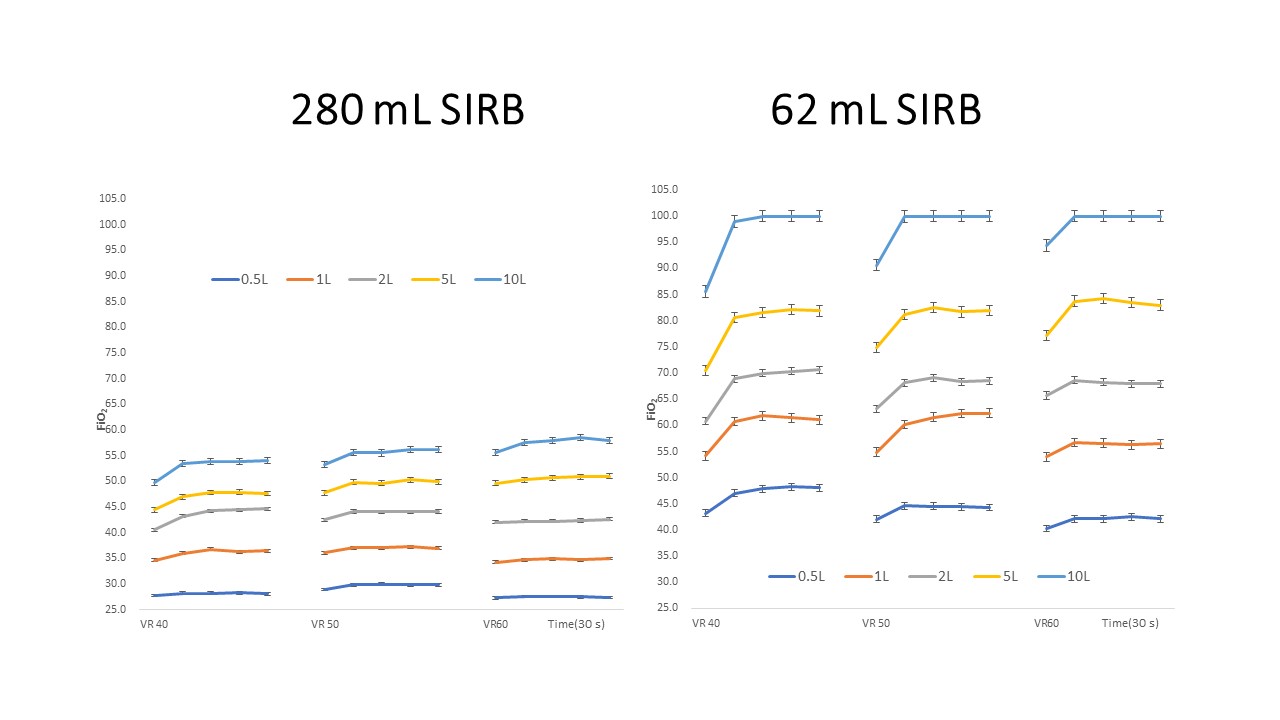 Interaction of panel plots among the SIRB of 280 mL or 62 mL capacity, ventilation rates (VR), and oxygen flow rates (L/min) at ≥40 cm H₂O peak inspiratory pressure over time (150 sec).
Interaction of panel plots among the SIRB of 280 mL or 62 mL capacity, ventilation rates (VR), and oxygen flow rates (L/min) at ≥40 cm H₂O peak inspiratory pressure over time (150 sec).
