Infectious Diseases 2: Bacterial infections
Session: Infectious Diseases 2: Bacterial infections
626 - Mortality Differences Between Community-Onset and Hospital-Onset Methicillin-Susceptible Staphylococcus aureus Bacteremia in Pediatric Patients
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 626.5854
Fumiya Okazaki, Tokyo Metropolitan Children's Medical Center, fuchu city, Tokyo, Japan; Meiwa Shibata, Tokyo Metropolitan Children's Medical Center, Fuchu, Tokyo, Japan; Yuho Horikoshi, Tokyo metropolitan children's medical center, Fuchu, Tokyo, Japan

Fumiya Okazaki, MD (he/him/his)
Resident
Tokyo Metropolitan Children's Medical Center
fuchu city, Tokyo, Japan
Presenting Author(s)
Background: Methicillin-susceptible Staphylococcus aureus (MSSA) is a major cause of bacteremia in children, though comparative outcome data for community-onset versus hospital-onset MSSA bacteremia in pediatric patients are limited.
Objective: This study aimed to evaluate prognostic differences between community-onset and hospital-onset MSSA bacteremia in pediatric patients.
Design/Methods: A retrospective study was conducted at a pediatric hospital from March 2010 to September 2024. Pediatric patients were included with MSSA bacteremia, excluding recurrent episodes, polymicrobial samples, contaminants, and co-infection cases. Analyses were stratified by community or hospital onset to compare prognosis, underlying conditions, diagnoses, antimicrobial therapies, and adverse effects.
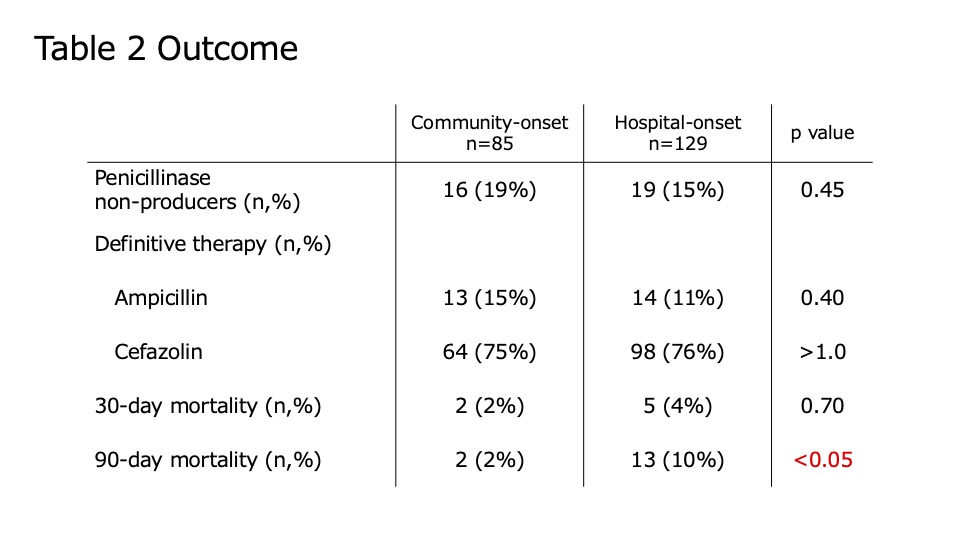
Results: Among 598 MSSA-positive samples, 214 met inclusion criteria, with 85 cases (41%) classified as community-onset and 129 (59%) as hospital-onset. In the community-onset group, 51% were male, median age 9 years (IQR: 2–12); the hospital-onset group included 64% males, median age 1 year (IQR: 0–10). Musculoskeletal (52%) and catheter-related infections (18%) were most common in community-onset cases, while catheter-related infections accounted for 53% of hospital-onset cases. Half of the community-onset group had no underlying disease, whereas hematologic diseases (16%), cardiovascular conditions (16%), and preterm birth (16%) were common in hospital-onset cases. Penicillinase non-producers/producers were 19%/76% in community-onset and 15%/78% in hospital-onset cases. Definitive therapy included ampicillin in 15% and cefazolin in 75% of community-onset cases, and ampicillin in 11% and cefazolin in 76% of hospital-onset cases. The 30-day mortality rate was 2% in community-onset and 4% in hospital-onset cases (p=0.70), while 90-day mortality was 2% and 10%, respectively (p < 0.05). Adverse effect rates were comparable between groups.
Conclusion(s): Thirty-day mortality was similar between community-onset and hospital-onset MSSA bacteremia in children; however, 90-day mortality was higher in hospital-onset cases, likely reflecting the greater prevalence of underlying conditions in this group.
Diagnoses clinically identified with as the cause of bacteremia
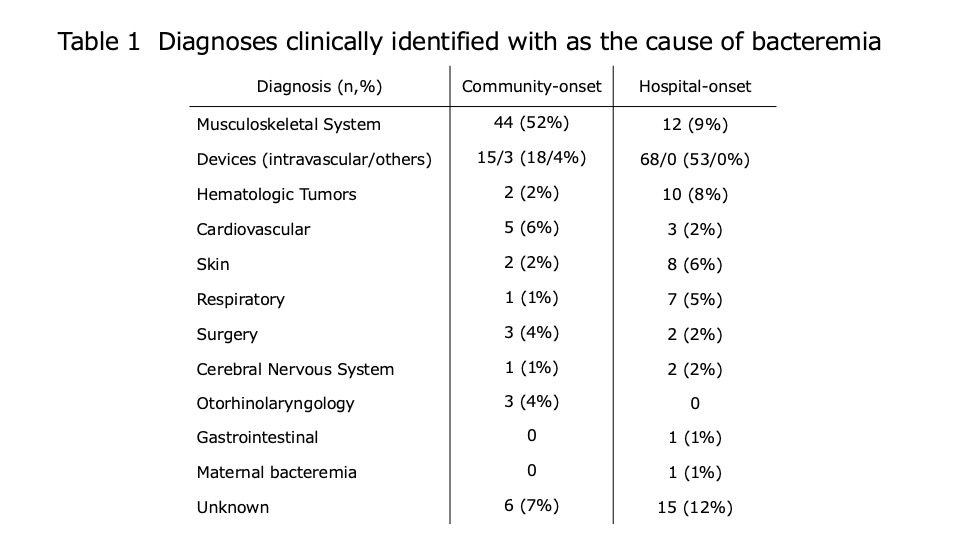
Outcome