Pulmonology
Session: Pulmonology
100 - Mesenchymal Stem Cell Therapy Prevents Airway Hyperreactivity in a Mouse Model of Neonatal Continuous Positive Airway Pressure
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 100.5872
Anusha Mopuri, UH Rainbow Babies & Children's Hospital, Beachwood, OH, United States; Morgan L.. Sutton, Case Western Reserve University, Chesterland, OH, United States; Thomas M. Raffay, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Catherine Mayer, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Richard Martin, Case Western Reserve University School of Medicine, Cleveland, OH, United States; Michael Konstan, Case Western Reserve University School of Medicine, Akron, OH, United States; Peter M. MacFarlane, Case Western Reserve University School of Medicine, Cleveland, OH, United States
- AM
Anusha Mopuri, MBBS, MD (she/her/hers)
Pediatric Pulmonology Fellow
UH Rainbow Babies & Children's Hospital
Beachwood, Ohio, United States
Presenting Author(s)
Background: RATIONALE: Bronchopulmonary dysplasia (BPD) is a chronic lung disease of premature infants and the most common complication of prematurity, affecting about one third of infants born less than 1.5kg and less than 29 weeks gestational age in the U.S. annually. Current practice favors treating neonatal respiratory distress with non-invasive ventilation, including continuous positive airway pressure (CPAP), over ventilation that requires endotracheal intubation. However, CPAP use has unintended consequences in premature infants and has been recently proposed to contribute to airway hyper reactivity (AHR) and wheezing disorders in childhood. Human mesenchymal stem cells (hMSCs) have begun to show promise as a therapeutic treatment for BPD, but its benefits to lung function following CPAP are unknown.
Objective: To test the hypothesis that neonatal CPAP-induced airway reactivity can be prevented by aerosolizing conditioned media from bone-marrow-derived hMSC cultures in an established neonatal mouse model.
Design/Methods: Neonatal mice were fitted with a custom-made mask to deliver CPAP (6cmH2O, 3 h/day) daily for the first 7 postnatal days. Mice also received 1 h administration of aerosolized (5ml) conditioned media (50% Rooster media in saline) immediately prior to each CPAP session. The conditioned media was obtained from a single human donor from which bone-marrow-derived hMSCs were incubated for 72h. On day 21, measurements of airway reactivity to methacholine were made in vitro using the precision lung slice preparation (PCLS) to assess the magnitude of AHR. Statistical analysis on AHR was performed using a repeated measures ANOVA to assess for differences in the slope of the response to increasing doses of methacholine.
Results: CPAP resulted in AHR to methacholine compared to untreated control mice (p < 0.05), which was prevented by aerosolization of hMSC-conditioned media (hMSC-CM; Fig. 1). There was no effect of un-conditioned hMSC media (UCM) on CPAP-induced AHR.
Conclusion(s): These data suggest that conditioned media used to culture hMSCs may be a promising therapy to prevent later AHR in former preterm infants who required prior CPAP administration. Studies are underway to determine the mechanistic benefits of hMSC against AHR and lung remodeling.
Fig. 1. Airway responses to methacholine challenge using the in vitro living lung slice preparation from 21-day old male mice with or without (Control) prior CPAP exposure between P 1-7 days of age.
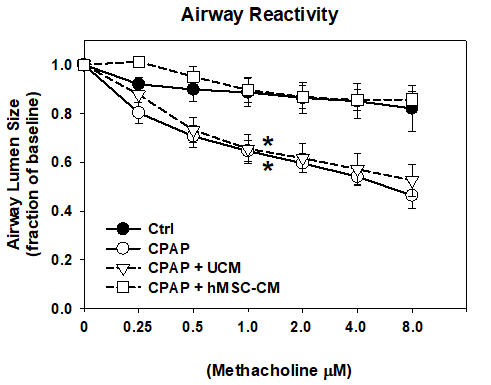 Mice received aerosolized hMSC conditioned media (hMSC-CM) or unconditioned media (UCM) prior to each CPAP session. Airway reactivity was quantified as a change in airway lumen area to increasing doses of methacholine. Data are expressed as a fraction of baseline. Data are means +/-1SEM. *sig. diff. in slopes vs Control and CPAP+hMSC-CM group, p<0.05. Repeated measures ANOVA, N=12-20 airways/treatment group.
Mice received aerosolized hMSC conditioned media (hMSC-CM) or unconditioned media (UCM) prior to each CPAP session. Airway reactivity was quantified as a change in airway lumen area to increasing doses of methacholine. Data are expressed as a fraction of baseline. Data are means +/-1SEM. *sig. diff. in slopes vs Control and CPAP+hMSC-CM group, p<0.05. Repeated measures ANOVA, N=12-20 airways/treatment group. 
