Neonatal Neurology 3
Session: Neonatal Neurology 3
365 - Height of maternal fever during labor is associated with an increased risk of hypoxic-ischemic encephalopathy and adverse neonatal outcomes
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 365.5173
Marie Cornet, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; MICHAEL W. KUZNIEWICZ, Kaiser Permanante, Los Gatos, CA, United States; Aditi Lahiri, Kaiser Permanente, Division of Research, Berkeley, CA, United States; Aaron W. Scheffler, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Yvonne W. Wu, UCSF, San Francisco, CA, United States
- MC
Marie Cornet, MD, PhD (she/her/hers)
Assistant Professor
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Maternal fever occurs in up to 10% of laboring mothers. It is associated with adverse maternal and neonatal outcomes such as low Apgar scores, respiratory distress, sepsis, meconium aspiration syndrome, and death. Few studies have investigated the dose-response relationship between height and duration of maternal fever and neonatal neurologic outcomes.
Objective: To examine if the height of fever and/or duration between maternal fever onset and delivery modifies the risk of hypoxic-ischemic encephalopathy (HIE) and whether this association persists after adjusting for the duration of labor.
Design/Methods: Population-based cohort study of singleton neonates without congenital anomalies born > 35 weeks at 15 Kaiser Permanente Northern California hospitals (January 2012 - July 2019). Births by elective cesarean section were excluded. Maternal fever was defined as at least one temperature >38°C before delivery. Maximal maternal temperature and timing of the first maternal fever were extracted from medical records. HIE was defined as the presence of neonatal encephalopathy and perinatal acidosis (cord pH < 7 or base deficit >10 within 2 hours after birth). Secondary outcomes included therapeutic hypothermia, seizures, acidosis, 5-min Apgar score < 7, early onset sepsis, and neonatal unit admission. We evaluated the associations between maximal maternal temperature and duration between fever onset to delivery and neonatal outcomes, using Poisson regression with robust standard error clustered by hospital, adjusting for duration of labor as a spline.
Results: Among 248,594 laboring mothers, 25,760 (10.4%) had fever, and their characteristics are de-scribed in Table 1. HIE occurred in 487 neonates (0.20%). The incidence of HIE was higher among infants of febrile compared to afebrile mothers (Relative risk - RR 3.0 [95% CI 2.6-3.5]). Both the height (Figure 1A) and duration (Figure 1B) of fever were associated with increased risk of HIE. After adjusting for duration of labor, the incidence of HIE increased with each 0.1°C in-crease in maximal maternal temperature (RR 1.09; 95% CI 1.08-1.11) and for each hour between fever onset and delivery (RR 1.06 95%CI 1.05-1.07). The incidence of all secondary outcomes al-so increased with increasing height of maternal temperature (Table 2).
Conclusion(s): The higher the maternal fever and the longer the duration between fever onset and delivery, the higher the risk of developing HIE. Novel strategies designed to predict the risk of adverse neonatal outcomes during labor and delivery should account for these factors.
Table 1: Maternal and infant characteristics among a cohort of 248,594 mother-infant dyads stratified by exposure to maternal fever
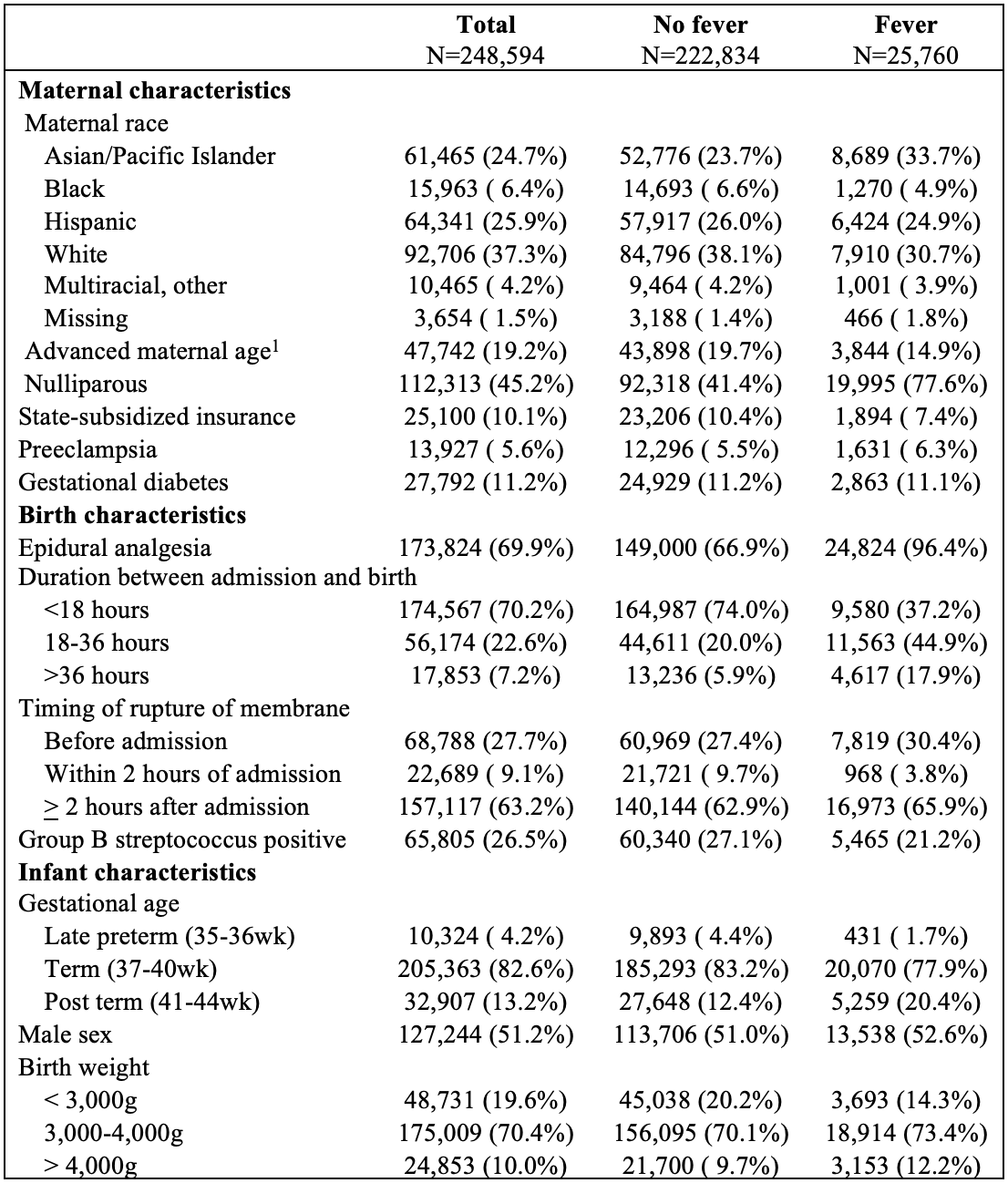 1. Maternal age>35 years old
1. Maternal age>35 years oldTable 2: Incidence and relative risks of HIE and secondary outcome by maximal maternal temperature in labor
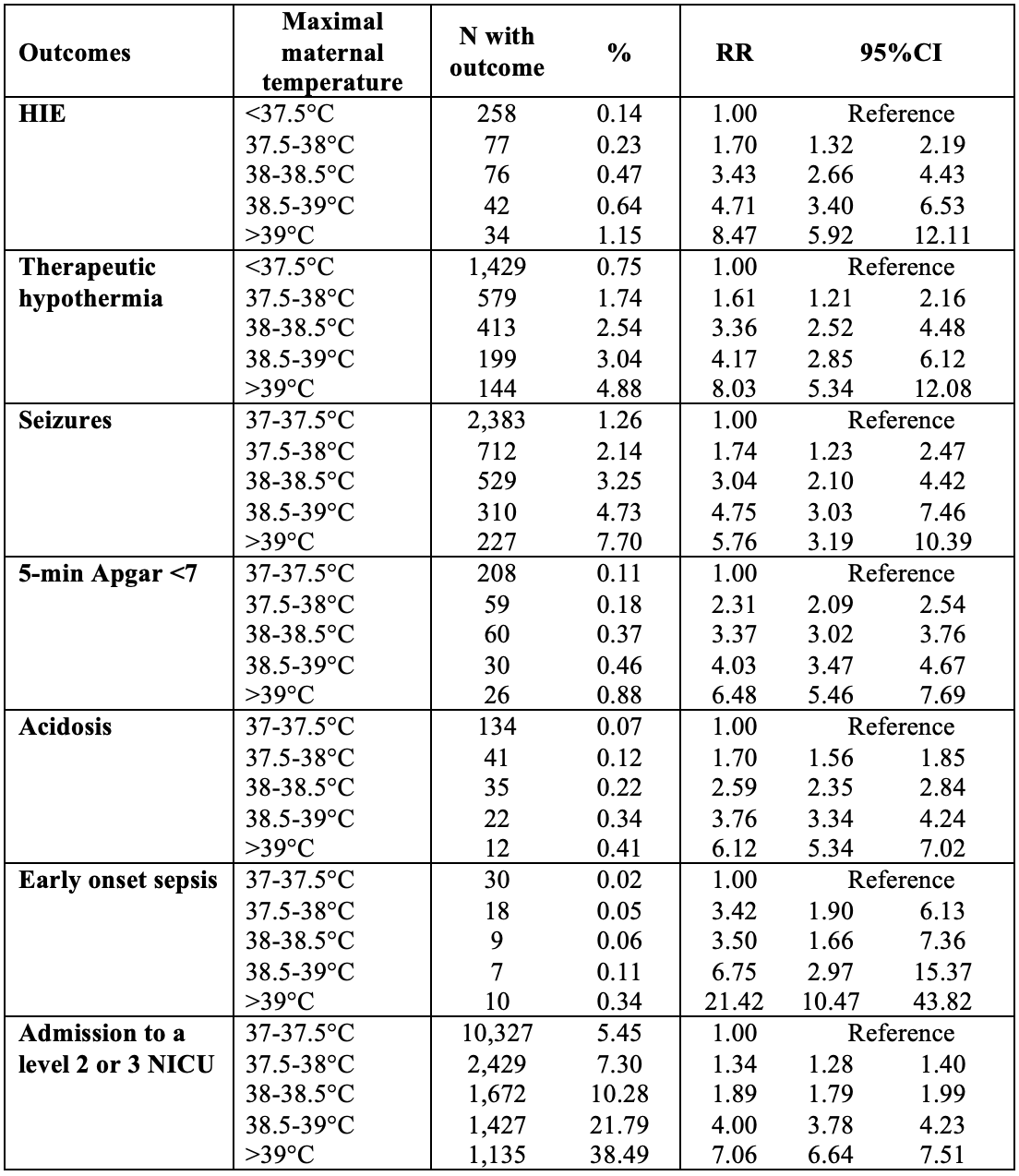 HIE: Hypoxic ischemic encephalopathy NICU: Neonatal intensive care unit
HIE: Hypoxic ischemic encephalopathy NICU: Neonatal intensive care unitFigure 1: Incidence of HIE and 95% CI based on height (A) and duration (B) of fever during labor.
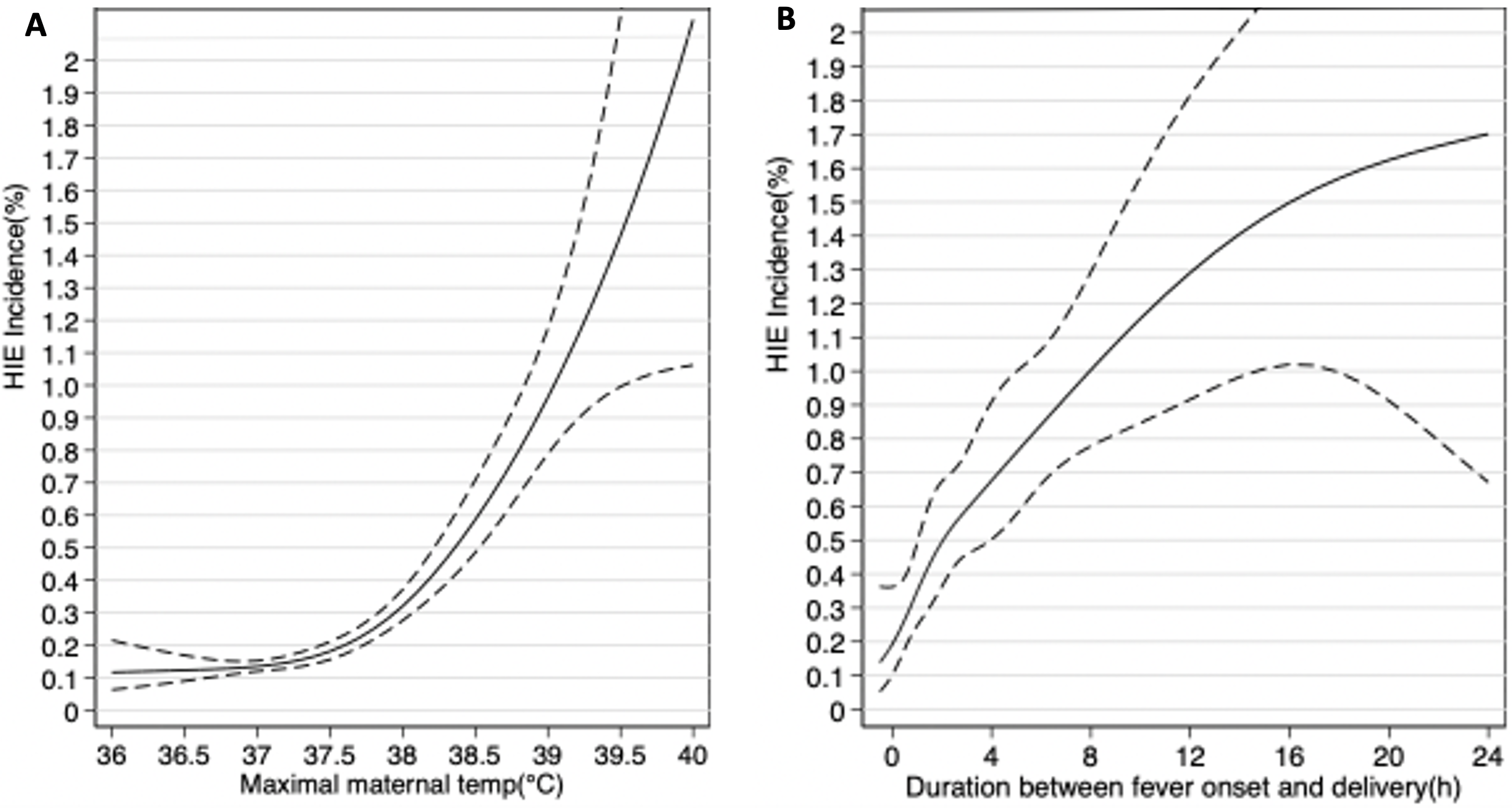 Estimations obtained by logistic regression modeling transforming predictor variables (maximal maternal temperature and duration between fever onset and delivery) as restricted cubic splines.
Estimations obtained by logistic regression modeling transforming predictor variables (maximal maternal temperature and duration between fever onset and delivery) as restricted cubic splines. Table 1: Maternal and infant characteristics among a cohort of 248,594 mother-infant dyads stratified by exposure to maternal fever
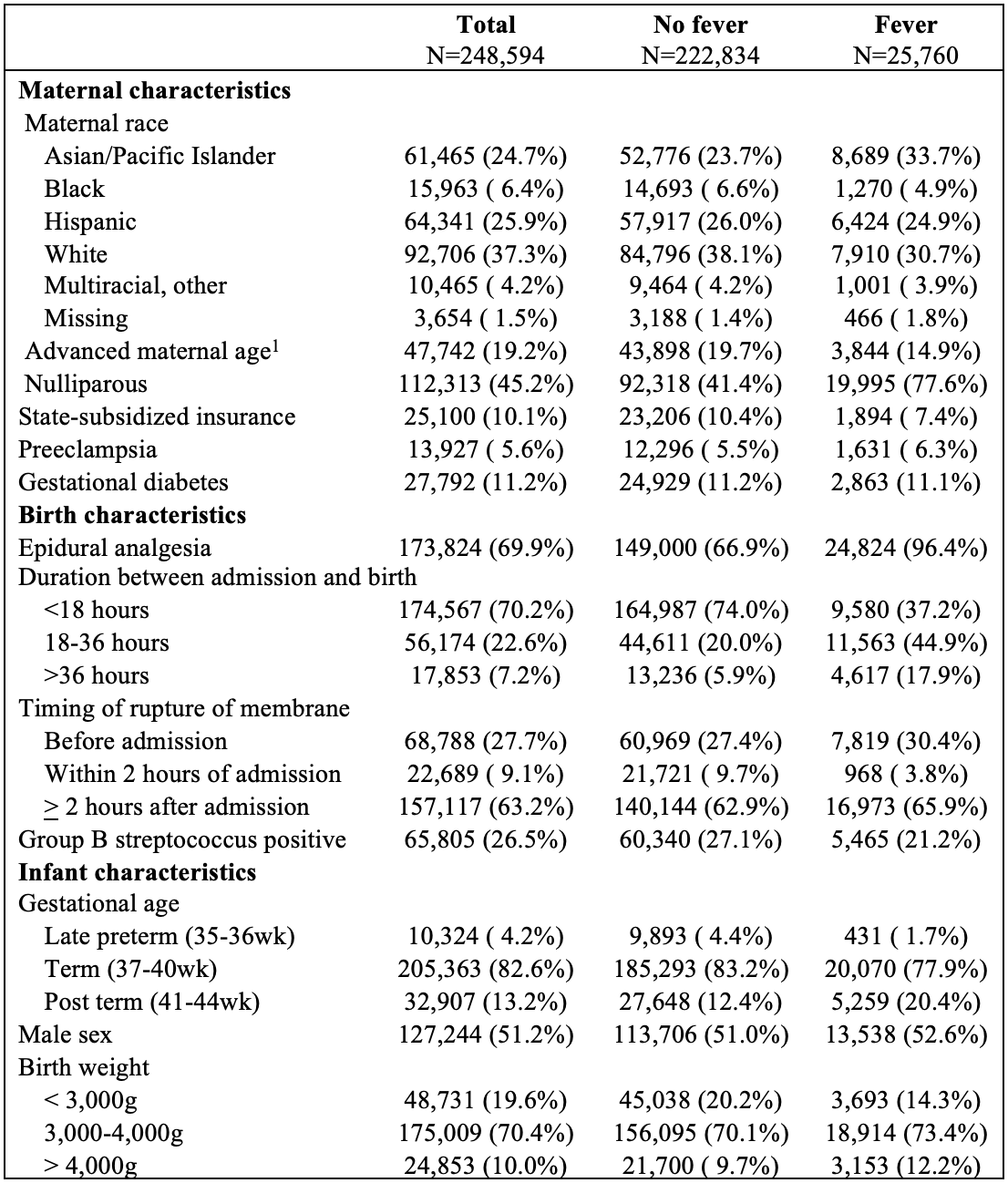 1. Maternal age>35 years old
1. Maternal age>35 years oldTable 2: Incidence and relative risks of HIE and secondary outcome by maximal maternal temperature in labor
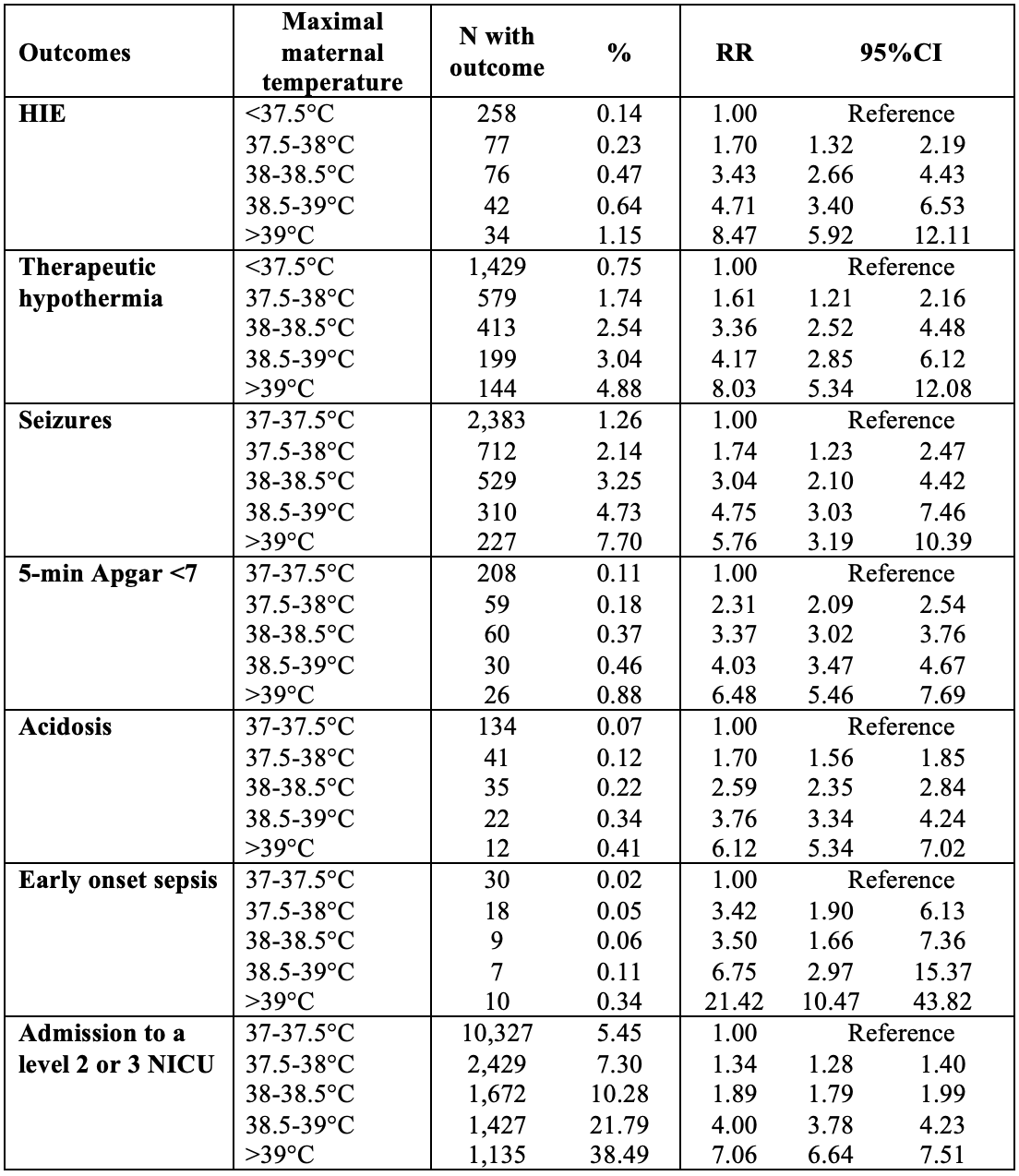 HIE: Hypoxic ischemic encephalopathy NICU: Neonatal intensive care unit
HIE: Hypoxic ischemic encephalopathy NICU: Neonatal intensive care unitFigure 1: Incidence of HIE and 95% CI based on height (A) and duration (B) of fever during labor.
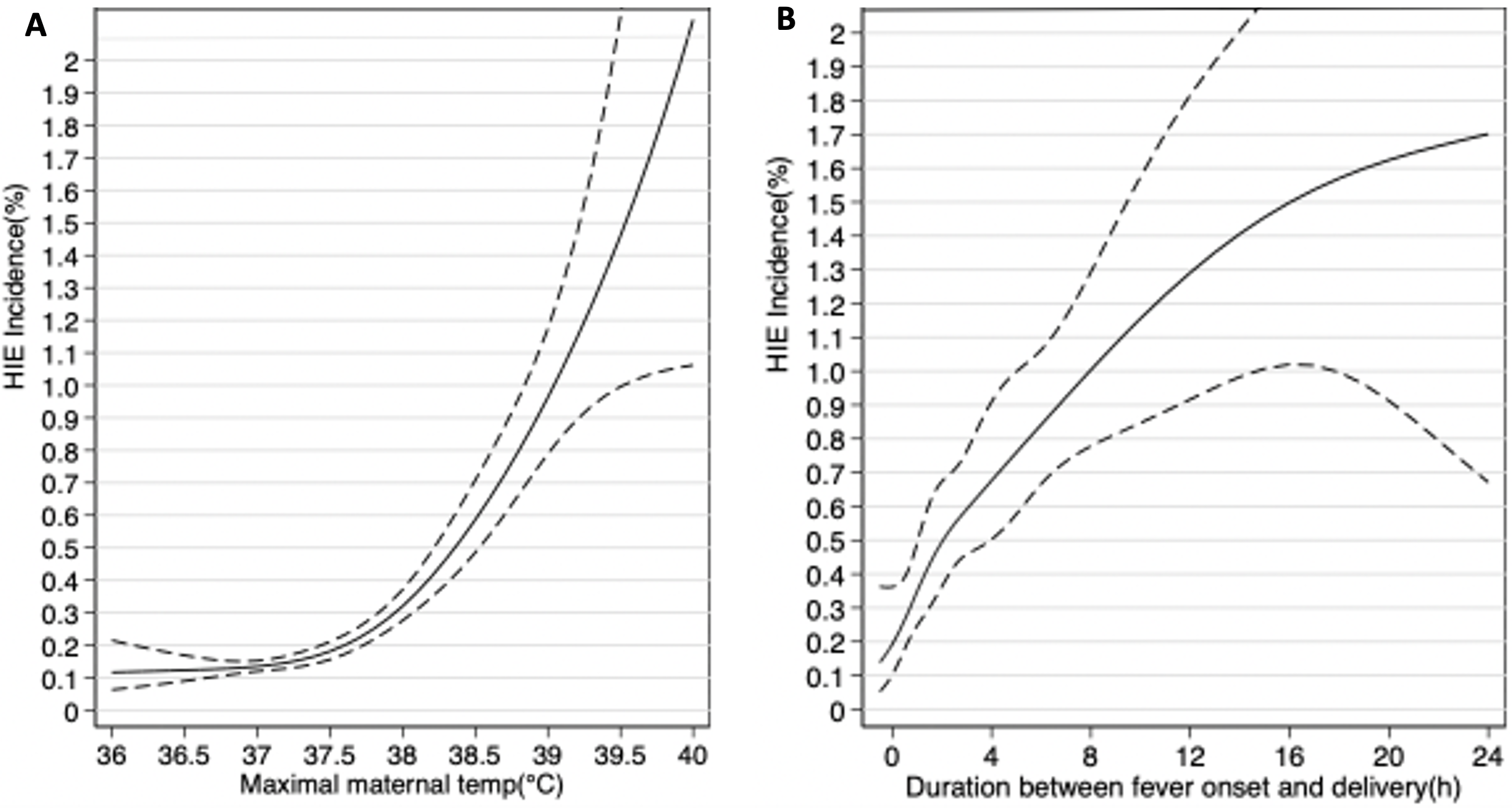 Estimations obtained by logistic regression modeling transforming predictor variables (maximal maternal temperature and duration between fever onset and delivery) as restricted cubic splines.
Estimations obtained by logistic regression modeling transforming predictor variables (maximal maternal temperature and duration between fever onset and delivery) as restricted cubic splines. 
