Immunizations/Delivery 1
Session: Immunizations/Delivery 1
668 - Influenza Vaccine Hesitancy among Youth and Caregivers of Youth with Sickle Cell Disease
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 668.5232
Joseph Walden, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Joseph Stanek, Nationwide Childrens Hospital, Columbus, OH, United States; Megan Griffith, Nationwide Children's Hospital, Columbus, OH, United States; Leena Nahata, Ohio State University College of Medicine, Columbus, OH, United States; Susan Creary, Nationwide Children's Hospital, Columbus, OH, United States
- JW
Joseph Walden, BS (he/him/his)
Medical Student
University of Cincinnati College of Medicine
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Sickle cell disease (SCD) is a blood disorder predominantly affecting minority populations. Youth with SCD are at risk for severe infections and influenza-related hospitalizations. Vaccination is the best prevention, yet rates have declined among children nationally. Beyond access barriers, vaccine hesitancy may contribute. However, there are limited contemporary data exploring influenza vaccine hesitancy among youth with SCD and their caregivers.
Objective: To describe influenza vaccine hesitancy among adolescents and young adults (AYA) and caregivers (CG) of children with SCD and determine if vaccine hesitancy is associated with socioeconomic markers and vaccination status.
Design/Methods: AYA (≥14 years) with SCD and CG of youth (aged 6 months-17 years) with SCD were recruited from hematology clinics at Nationwide Children's Hospital (March – April 2024). A modified version of the validated World Health Organization’s Vaccine Hesitancy Scale (VHS) was administered. Likert-style item responses range from 1-4. Mean scores were calculated from the eight VHS items to quantify hesitancy. Lower scores indicated greater hesitancy. Demographic information (i.e., age, race) was self-reported. Influenza vaccination status for AYA and children of CG during the 2023-2024 influenza season was abstracted from the electronic health record. Kruskal–Wallis and Wilcoxon rank-sum tests compared VHS scores by socioeconomic markers (i.e., insurance, education) among CG and by vaccination status among all participants.
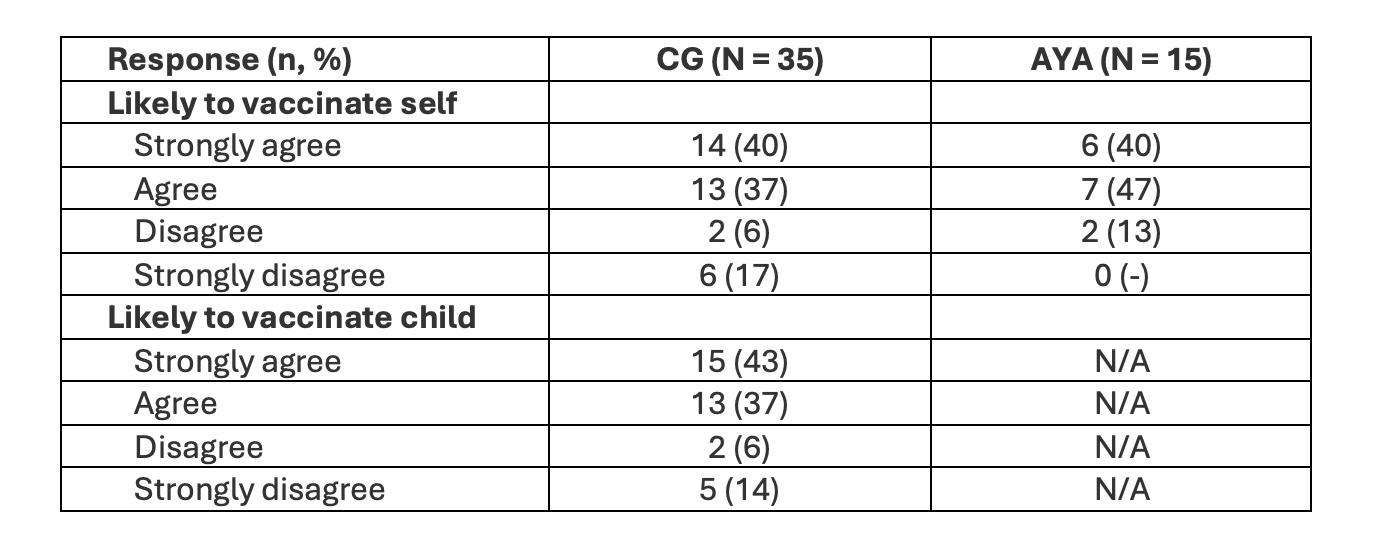
Results: Mean CG (n=35) VHS score was 2.94 compared to 3.02 for AYA (n=15) (p=0.53, Table and Figure 1). Most CG (77%) and AYA (87%) reported that they intended to get themselves vaccinated (p=0.70) (Table 2). Mean CG VHS score was significantly lower for those with publicly insured children versus those with privately insured children (2.68 vs. 3.28, p=0.035) but did not significantly differ by CG age (p=0.84), birthplace (p=0.41), or education level (p=0.09).
Regarding vaccination status, 25% of youth with SCD (AYA or children of CG subjects) were unvaccinated. Mean VHS score for those who were (or whose child was) unvaccinated was significantly lower than those who were (or whose child was) vaccinated (2.15 vs. 3.23, p< 0.001).
Conclusion(s): Our data suggest that influenza vaccination gaps persist among youth with SCD. Interventions to specifically address vaccine hesitancy may be warranted, especially among unvaccinated and publicly insured youth with SCD. Future work is needed to elucidate factors that drive influenza vaccine hesitancy and decision-making among this vulnerable population.
Table 1. Participant Demographics
.jpg)
Figure 1. Modified VHS Responses
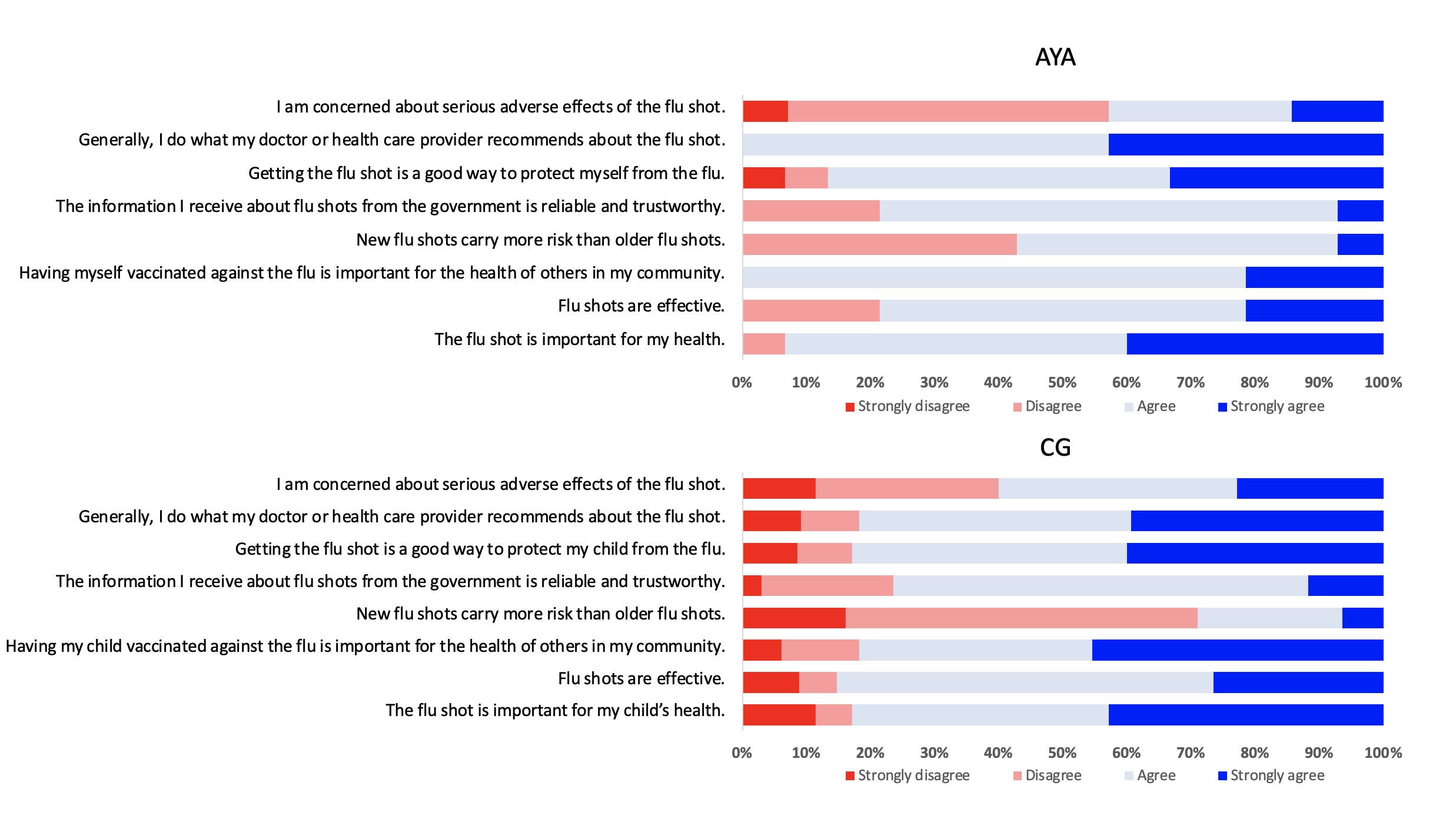
Table 2. Participant Intention to Vaccinate