Neonatal/Infant Resuscitation 1
Session: Neonatal/Infant Resuscitation 1
286 - Respiratory function monitoring and visual attention in the resuscitation of term infants; A Mannequin based randomised crossover trial
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 286.6405
Robert Joyce, Cork University Maternity Hospital, Dublin, Dublin, Ireland; Dalal Alhassan, Cork University Maternity Hospital (CUMH), Schull, Cork, Ireland; Anne L. Murray, University College Cork, Cork, Cork, Ireland; Aisling Fanning, Cork University Maternity Hospital, Cork, Cork, Ireland; Vicki Livingstone, University College Cork, Cork, Cork, Ireland; Mmoloki Kenosi, University College Cork, Cork, Cork, Ireland; Eugene M. Dempsey, University College Cork, Cork, Cork, Ireland

Robert Joyce, MRCPI MB BCh BAO
Neonatal Specialist Registrar
Cork University Maternity Hospital
Dublin, Dublin, Ireland
Presenting Author(s)
Background: Approximately 10% of infants will require some form of intervention at delivery, with 6% requiring positive pressure ventilation (PPV) via a mask. The Neonatal Resuscitation Programme (NRP) stipulates the provision of 30 seconds of effective uninterrupted PPV prior to the escalation of support. A Respiratory Function Monitor (RFM) may assist providers in reaching this 30 seconds in a more timely fashion.
Objective: Primary
Determine the effect of RFM use on the amount of time required for operators to provide 30 seconds of effective PPV in a simulated term resuscitation.
Secondary
Assess the focus of operator visual attention (VA) during the simulation, and how this correlates with the provision of effective PPV both with and without a visible RFM.
Design/Methods: This was a randomised crossover trial conducted at Cork University Maternity Hospital (Cork, Ireland). Participants performed two simulated term resuscitations in random order during which they were tasked with providing 30 seconds of effective PPV to a term mannequin (Newborn Anne, Laerdal Medical, USA) with and without a RFM (Monivent, Sweden) visible to them. During each simulation a Holens headset (Microsoft, USA) was worn to assess the VA of the participants.
Results: Thirty clinicians of varying role and experience were enrolled and completed both simulations (n=30). Data was incomplete for two participants in the RFM arm; one for whom the RFM data could not be retrieved, and another for whom VA could not be analysed. Sixteen participants completed their first attempt without the RFM visible (53.3%).
Only one participant did not complete the task with the RFM not visible (96.7% successful); all participants completed the task when the RFM was visible (100%).
The median time taken to provide 30 seconds of effective PPV when the RFM was not visible was 73.1 (IQR 53.9, 106.1) seconds compared to 72.5 (IQR 46.7, 113.2) seconds (p=0.29) with the RFM visible. There was no significant difference in mean tidal volume provided between the two arms. There was a significant reduction in mask leak when the RFM was visible compared to when it wasn’t (p=0.033). The median percentage VA spent on the mannequin for the duration of the simulation decreased from 81.3% without the RFM visible, to 58.5% with the RFM visible (p < 0.001).
Conclusion(s): Less time is spent looking at the mannequin and there is an improvement in mask leak when utilising an RFM. However, having a RFM visible did not decrease the time taken to provide 30 seconds of effective PPV to a term mannequin in a simulated resuscitation, and nor did it increase administered tidal volumes.
Table 1
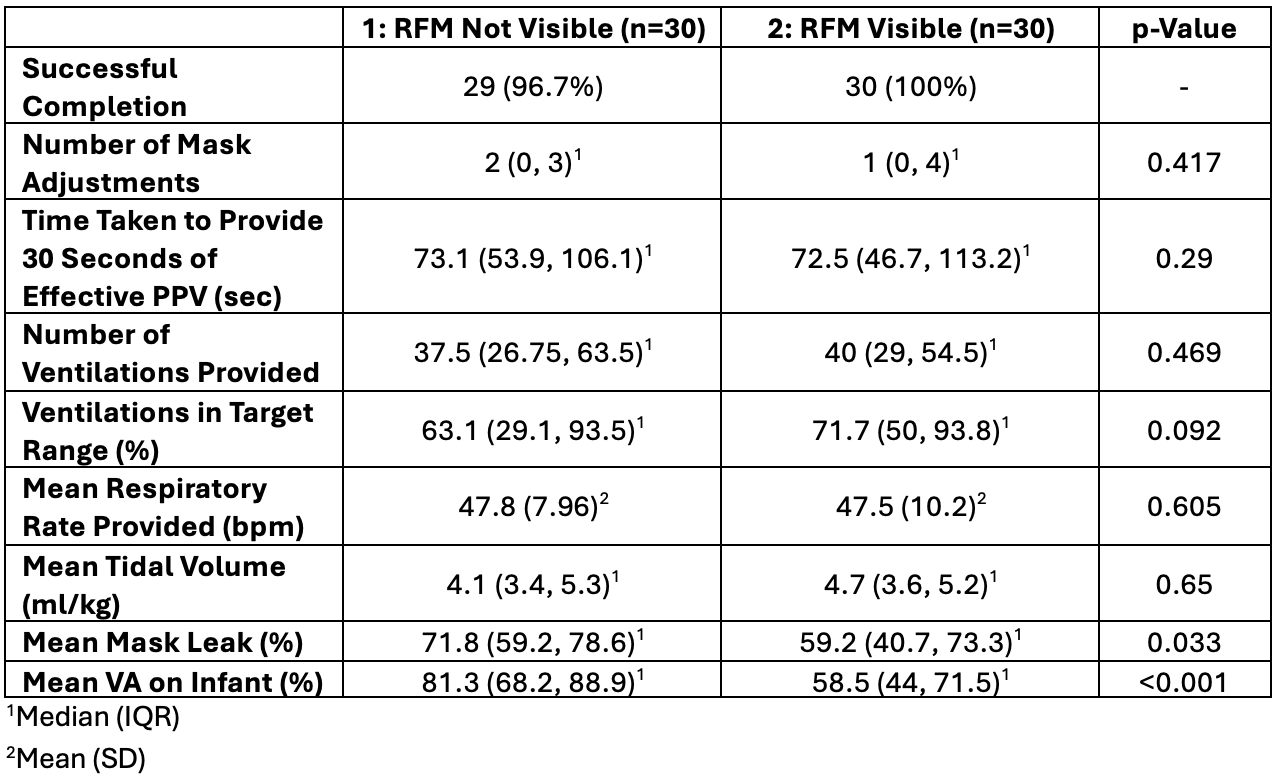 Results
Results
