Neonatal/Infant Resuscitation 2
Session: Neonatal/Infant Resuscitation 2
301 - Saline Bolus over 5 Minutes is Associated with High Risk of Post-ROSC Secondary Arrest in an Ovine Model of Hemorrhagic Arrest
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 301.6375
Rebecca Valdez, University of California Davis, Davis, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Amy Lesneski, University of California, Davis, School of Medicine, Davis, CA, United States; Victoria Hammitt, University of California, Davis, School of Medicine, Sacramento, CA, United States; Michelle J. Lim, University of California, Sacramento, CA, United States; Jessa Rose A. Li, University of California Davis Children's Hospital, Sacramento, CA, United States; Erin Riley, University of California, Davis, School of Medicine, Redding, CA, United States; Erika N.. Zerda, University of California, Davis, School of Medicine, Sacramento, CA, United States; Paulina Hume, University of California Davis Children's Hospital, 612 El Dorado Way, CA, United States; Sylvia Bowditch, University of California Davis Children's Hospital, Sacramento, CA, United States; Payam Vali, University of California, Davis, School of Medicine, sacramento, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States

Rebecca Valdez, B.S. (she/her/hers)
Trainee
University of California Davis
Davis, California, United States
Presenting Author(s)
Background: Fetal blood loss (e.g. feto-maternal hemorrhage) is a common cause of perinatal asphyxia. Neonatal signs of blood loss are variable ranging from being asymptomatic to shock and lack of response to epinephrine. Current Neonatal Resuscitation Program guidelines recommend administration of a volume expander infused over 5-10 minutes if the baby is not responding to the steps of resuscitation and there are signs of shock or a history of acute blood loss. It is not known if a faster bolus over 2-min may improve outcomes.
Objective: To compare the incidence of and time to return of spontaneous circulation (ROSC) between epinephrine followed by (1) saline bolus over 5-min vs (2) saline bolus over 2-min vs (3) no bolus after epinephrine in a model of hemorrhagic hypovolemic neonatal cardiac arrest.
Design/Methods: Term (~140d) fetal lambs were intubated and instrumented. Exsanguination (45-mL/kg of estimated weight) was followed by cord occlusion to induce hypovolemia and cardiac arrest. Following 5 min of asystole, lambs resuscitated with ventilation and chest compressions were randomized to neonatal CPR with umbilical venous epinephrine, followed by a 1) 10-mL/kg saline bolus over 5 min, 2) 10-mL/kg saline bolus over 2 min, and 3) no saline bolus. Hemodynamics and blood gases were monitored.
Results: Baseline characteristics and incidence of and time to ROSC were not different between the groups. There was no difference in carotid artery blood flow, mean blood pressure and heart rate between 5-min bolus, 2-min bolus and no-bolus groups after ROSC (figure 1 and 2a). Following ROSC, systemic hypotension (mean BP < 35 mmHg) and anemia (Hb < 9g/dL) were observed warranting whole blood transfusion (83%, 100% and 67%) and saline boluses (67%, 75% and 50%) in the 5-min bolus, 2-min bolus and no bolus groups respectively. Cerebral regional oxygen saturation (CrSO2) was higher in the 2-min bolus group at ROSC but was higher in the no-bolus group between 5 and 60 min after ROSC (figure 2b). CrSO2 increased with every blood transfusion (figure 2c). 50% the lambs in the 5-min bolus group, 25% of the lambs in the 2-min bolus group and none in the no-bolus group rearrested requiring re-initiation of CPR.
Conclusion(s): There was no immediate benefit from rapid administration of fluid bolus during resuscitation in hemorrhagic ovine neonatal cardiac arrest. During the post-ROSC phase, careful clinical assessment of hemodynamics is critical due to potential need for further volume expansion and risk of cardiac arrest. The effect of rapid saline bolus in the post-ROSC phase on a post-arrest ischemic heart needs further evaluation.
Comparison of baseline characteristics and ROSC outcomes between lambs in hypovolemic cardiac arrest that received 10mL/kg normal saline bolus over 5 min vs 2 min vs no bolus
.jpg)
Comparison of left carotid artery blood flow, mean blood pressure, and heart rate during exsanguination, resuscitation, and after ROSC among lambs that received 10mL/kg bolus during resuscitation over 5 min vs 2 min vs no bolus.
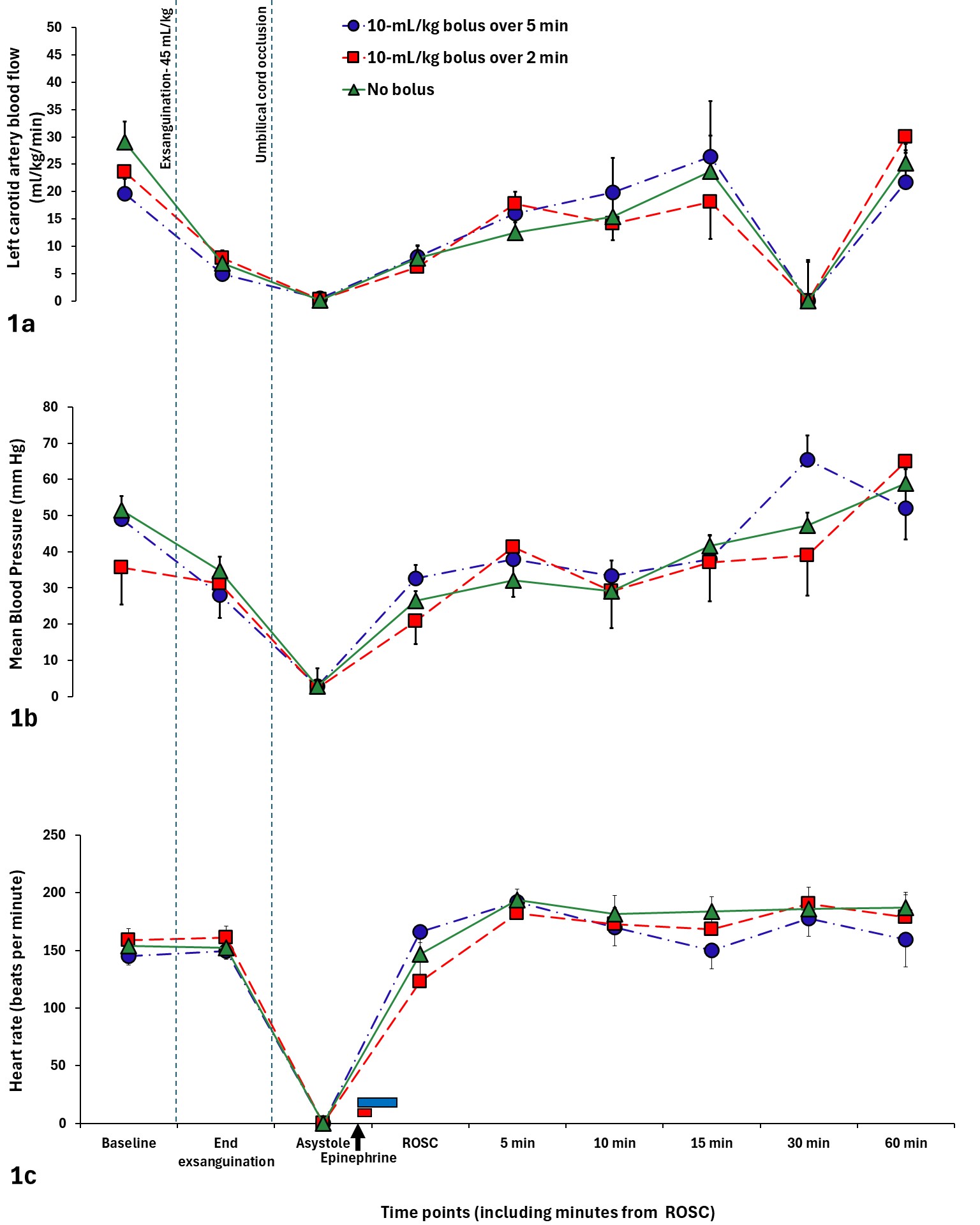 Carotid artery blood flow and mean blood pressure decreased significantly during exsanguination with no difference in heart rate. After ROSC, there was no difference in carotid artery blood flow, mean blood pressure, and heart rate between 10mL/kg normal saline bolus over 5 min vs. 2 min vs. no bolus groups. The blue bar near the x-axis represents the 10mL/kg bolus over 5 min being administered and the red bar represents the 10mL/kg bolus being administered over 2 min Data was compared using repeated ANOVA.
Carotid artery blood flow and mean blood pressure decreased significantly during exsanguination with no difference in heart rate. After ROSC, there was no difference in carotid artery blood flow, mean blood pressure, and heart rate between 10mL/kg normal saline bolus over 5 min vs. 2 min vs. no bolus groups. The blue bar near the x-axis represents the 10mL/kg bolus over 5 min being administered and the red bar represents the 10mL/kg bolus being administered over 2 min Data was compared using repeated ANOVA. Figure 2a shows the change in left carotid artery blood flow during resuscitation and the effect of saline bolus between lambs that received 10mL/kg saline bolus over 5 min vs 2 min vs no bolus. Figure 2b demonstrates the change in cerebral regional mixed venous oxygen saturation(CrSO2) during exsanguination, resuscitation, and after ROSC. Figure 2c shows a significant increase in CrSO2 after every blood transfusion. The blue bar near the x-axis represents the 10mL/kg bolus over 5 min being administered and the red bar represents the 10mL/kg bolus being administered over 2 min.
.jpg)

