Back
Background: Over recent years, the admission rate of late preterm infants to neonatal intensive care units (NICU’s) has increased. Some neonates are transferred immediately to the NICU, however many are initially admitted to the nursery but subsequently require NICU transfer, a process that might delay initiation of appropriate therapeutic interventions and elevate the risk for complications. This highlights the need for early identification of infants at risk for NICU admission
Objective: To estimate and identify perinatal and postnatal risk factors associated with NICU admission among late preterm infants (gestational age 34–36 weeks)
Design/Methods: This retrospective cohort study analyzed electronic health records of late preterm infants (34–36 weeks gestational age) born in a single tertiary NICU between January 2020 and December 2023. Infants with congenital anomalies were excluded. Perinatal and postnatal factors associated with NICU admission were assessed and compared with those of infants admitted to the well-newborn nursery. Multivariable regression analysis was used to evaluate characteristics linked to NICU admissions
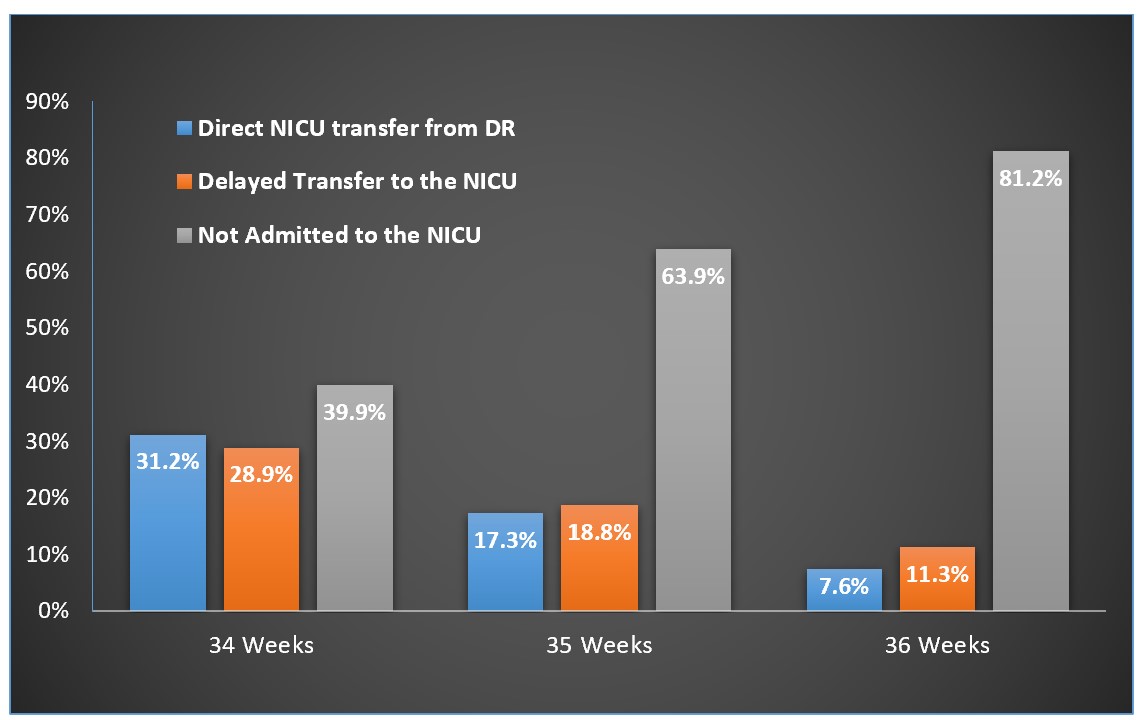
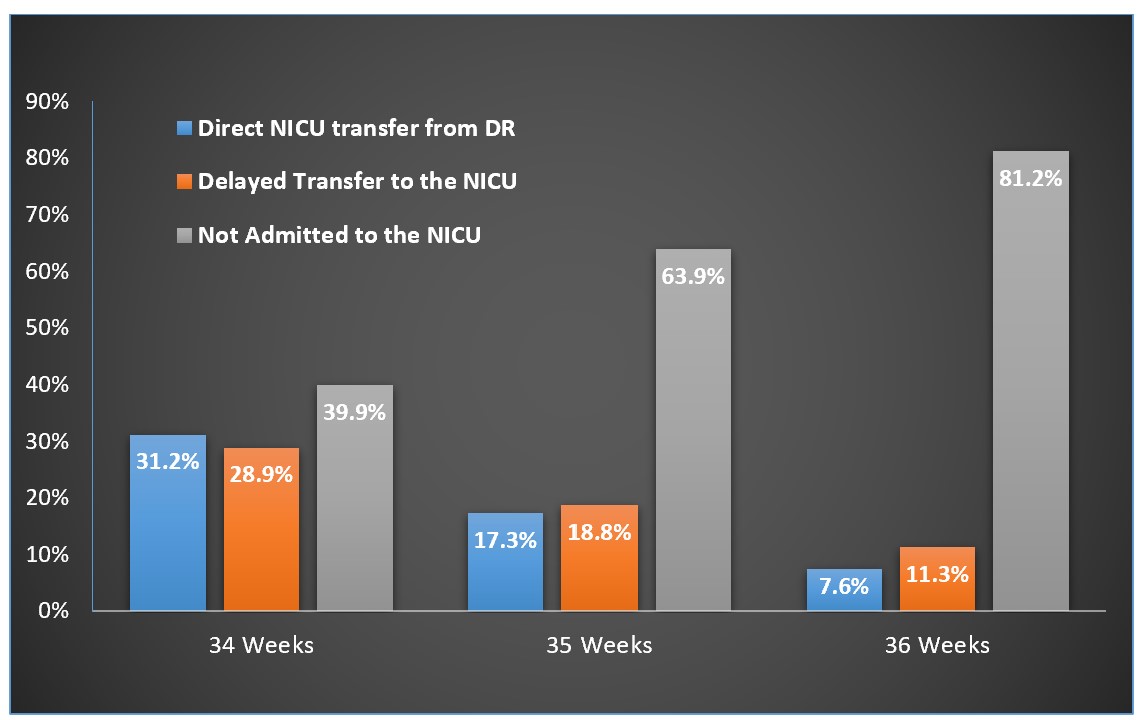
Results: Overall, 1674 infants: 207 (12.3%) 34-weeks Gestational age (GA), 401 (23.9%) 35-weeks GA, and 1066 (63.6%) 36-weeks GA. Figure 1 shows the admission rate of all late preterm infants. Figure 2 shows the cumulative admission rate of late preterm infants over time. The late admission rate of infants born at 34w, 35w, 36w gestation was 42%, 22% and 12%, respectively. Univariable analysis (Table 1) revealed that, Earlier GA (36w vs. 35w, p< 0.001), low birth weight ( < 2500gr) (46% vs. 59%, p< 0.001), longer maternal hospitalization prior to delivery (4.9 vs. 5.2 days, p=0.007) and Cesarean delivery (43.6% vs 56.8%, p< 0.001) were associated with a later transfer to NICU. Multivariable analysis showed association of the following factors with NICU admission: Increased GA (1 day increment) (OR=0.89, 95%CI: 0.87-0.911, p< 0.001), birth at night at night (OR=0.601, 95%CI 0.426-0.848, p< 0.004), multiple delivery (OR=0.668, 95%CI 0.499-0.895, p=0.007), and borderline significant in 5th minute APGAR score (OR=2.525, 95%CI 0.982-6.493, p=0.055).
Conclusion(s): Delayed NICU transfer of infants born at 34-36 weeks gestation, occurs commonly. Decrease GA increases the risk of late NICU admission. The “protective” effect of multiple delivery may be a true finding or maybe influenced by the attempt to keep twins together at the nursery. Further research is needed to assess the effect of delayed NICU transfer on neonatal outcomes.
Table 1: Description of Cohort of Infants Born at 34-35 Weeks’ Gestation.
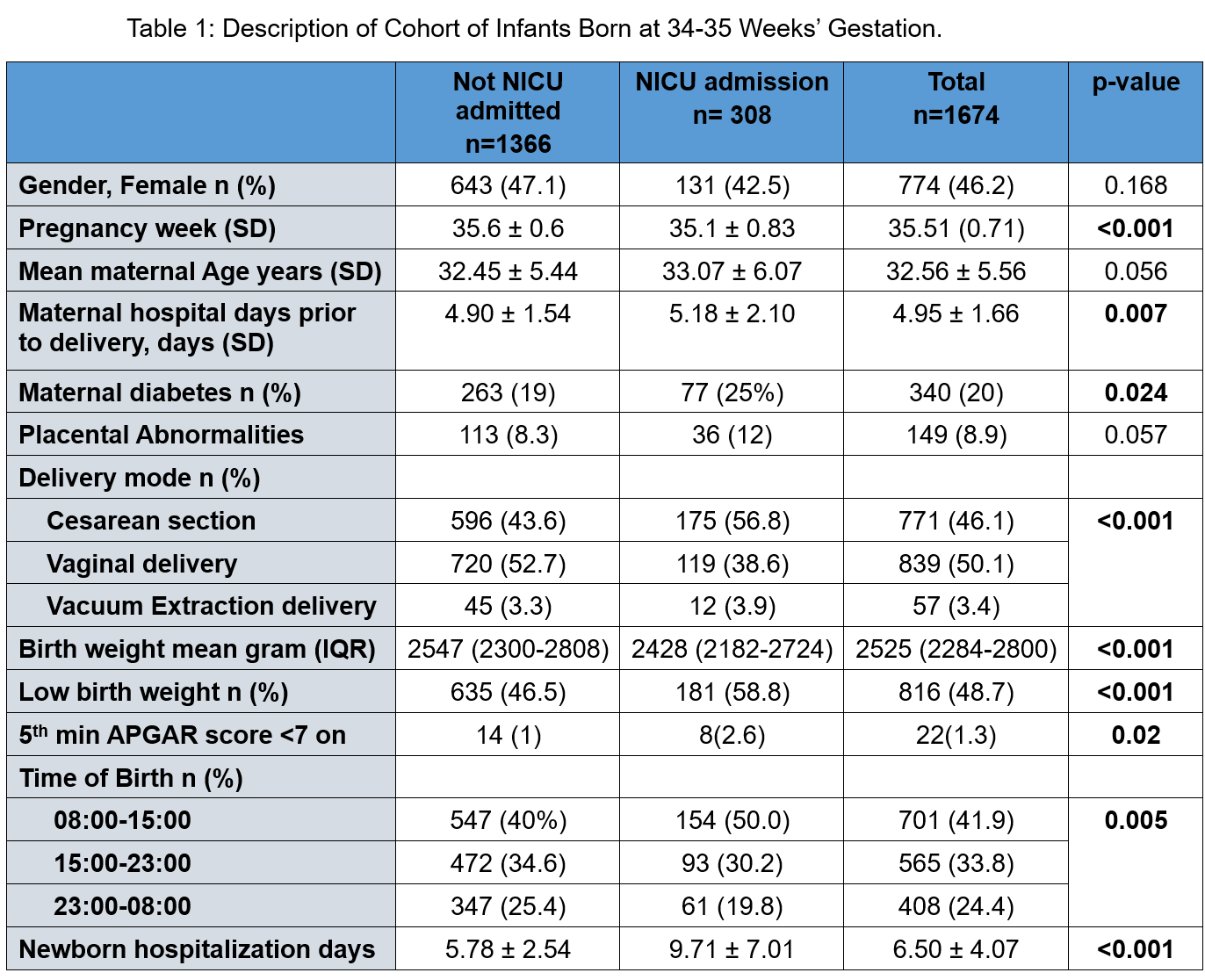
Figure 2: Cumulative Risk of Transfer to Neonatal Intensive Care Unit Among Preterm, By Gestational Week at Birth
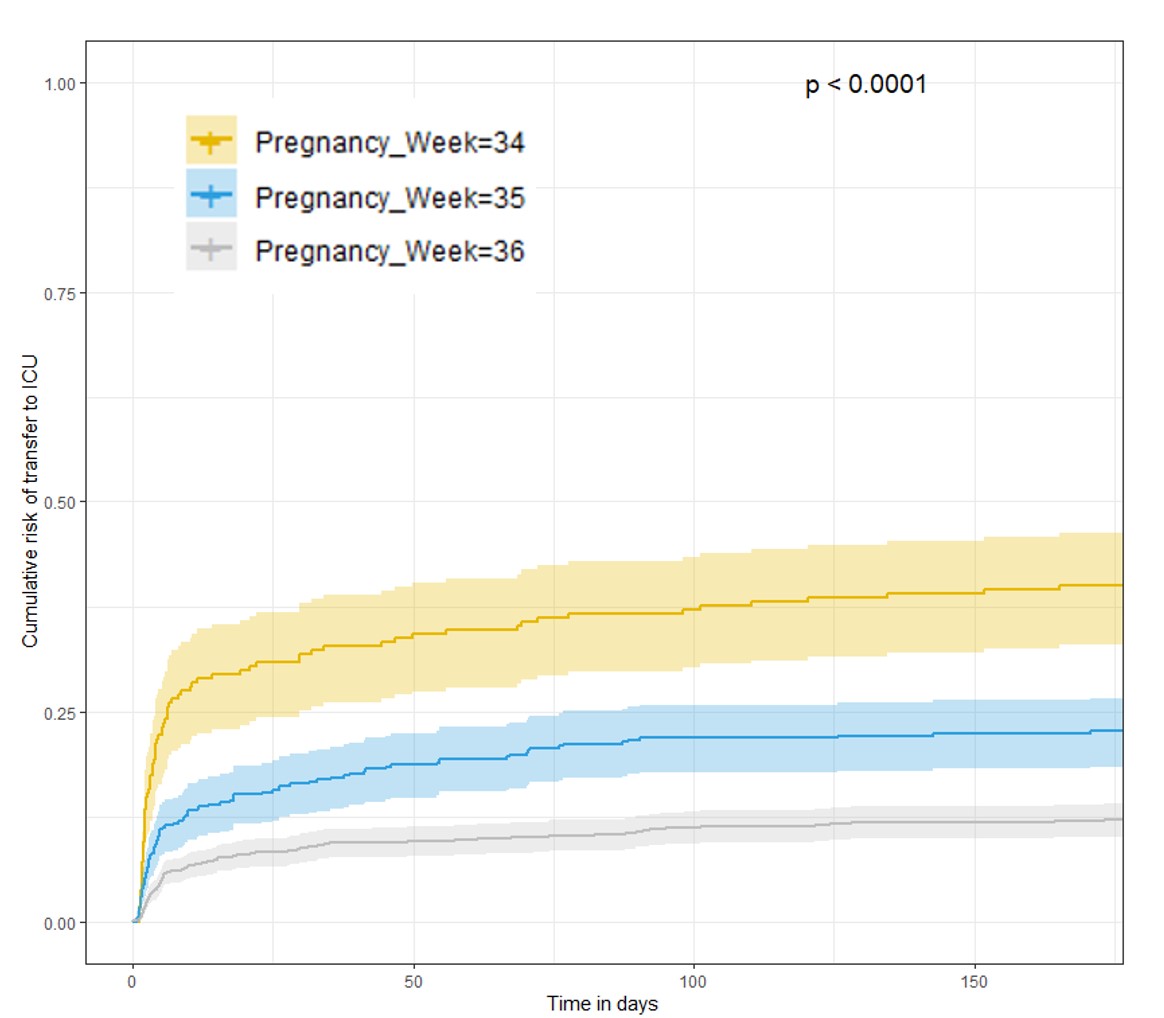
Figure 1: Neonatal intensive care unit admission rate of late preterm infants by gestational age.
Neonatal General 3: NICU Practices
Session: Neonatal General 3: NICU Practices
548 - Which Late Preterm Infants Should We Admit to the Neonatal Intensive Care Unit?
Friday, April 25, 2025
5:30pm – 7:45pm HST
Eyal Elron, Schneider Children`s Medical Center of Israel, Petah Tikva, HaMerkaz, Israel; Micky Osovsky, BEILINSON HOSPITAL, HOD HASHARON, HaMerkaz, Israel; Ruben Bromiker, Schneider children’s medical center of Israel, Petach Tikva, HaMerkaz, Israel; Nir Sokolover, Schneider children's medical center of Israel, Tel Aviv, Tel Aviv, Israel; Elena Segal, Schneider childrens hospital, Qiryat Ono, HaMerkaz, Israel; Tina Cris. Herscovici, Schneider Children’s Medical Center of Israel, Petah Tikva, HaMerkaz, Israel; Gabriel Chodick, Tel aviv university, Tel Aviv, Tel Aviv, Israel; Gil Klinger, Schneider Children's Medical Center of Israel and Tel Aviv University, Ramat Hasharon, HaMerkaz, Israel
- EE
Eyal Elron (he/him/his)
Neonatology fellow
Schneider Children`s Medical Center of Israel
Petah Tikva, HaMerkaz, Israel
Presenting Author(s)
Background: Over recent years, the admission rate of late preterm infants to neonatal intensive care units (NICU’s) has increased. Some neonates are transferred immediately to the NICU, however many are initially admitted to the nursery but subsequently require NICU transfer, a process that might delay initiation of appropriate therapeutic interventions and elevate the risk for complications. This highlights the need for early identification of infants at risk for NICU admission
Objective: To estimate and identify perinatal and postnatal risk factors associated with NICU admission among late preterm infants (gestational age 34–36 weeks)
Design/Methods: This retrospective cohort study analyzed electronic health records of late preterm infants (34–36 weeks gestational age) born in a single tertiary NICU between January 2020 and December 2023. Infants with congenital anomalies were excluded. Perinatal and postnatal factors associated with NICU admission were assessed and compared with those of infants admitted to the well-newborn nursery. Multivariable regression analysis was used to evaluate characteristics linked to NICU admissions
Results: Overall, 1674 infants: 207 (12.3%) 34-weeks Gestational age (GA), 401 (23.9%) 35-weeks GA, and 1066 (63.6%) 36-weeks GA. Figure 1 shows the admission rate of all late preterm infants. Figure 2 shows the cumulative admission rate of late preterm infants over time. The late admission rate of infants born at 34w, 35w, 36w gestation was 42%, 22% and 12%, respectively. Univariable analysis (Table 1) revealed that, Earlier GA (36w vs. 35w, p< 0.001), low birth weight ( < 2500gr) (46% vs. 59%, p< 0.001), longer maternal hospitalization prior to delivery (4.9 vs. 5.2 days, p=0.007) and Cesarean delivery (43.6% vs 56.8%, p< 0.001) were associated with a later transfer to NICU. Multivariable analysis showed association of the following factors with NICU admission: Increased GA (1 day increment) (OR=0.89, 95%CI: 0.87-0.911, p< 0.001), birth at night at night (OR=0.601, 95%CI 0.426-0.848, p< 0.004), multiple delivery (OR=0.668, 95%CI 0.499-0.895, p=0.007), and borderline significant in 5th minute APGAR score (OR=2.525, 95%CI 0.982-6.493, p=0.055).
Conclusion(s): Delayed NICU transfer of infants born at 34-36 weeks gestation, occurs commonly. Decrease GA increases the risk of late NICU admission. The “protective” effect of multiple delivery may be a true finding or maybe influenced by the attempt to keep twins together at the nursery. Further research is needed to assess the effect of delayed NICU transfer on neonatal outcomes.
Table 1: Description of Cohort of Infants Born at 34-35 Weeks’ Gestation.
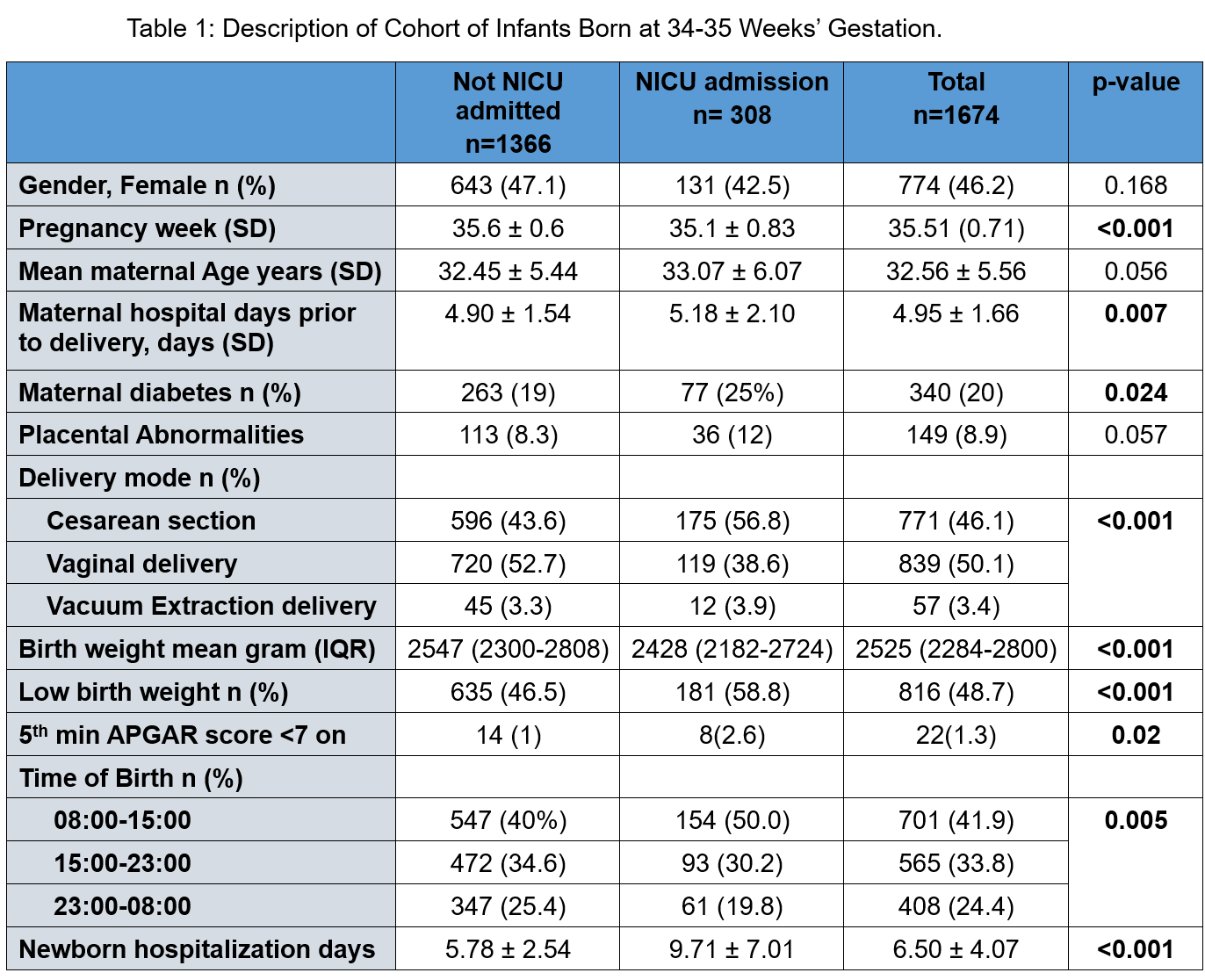
Figure 2: Cumulative Risk of Transfer to Neonatal Intensive Care Unit Among Preterm, By Gestational Week at Birth
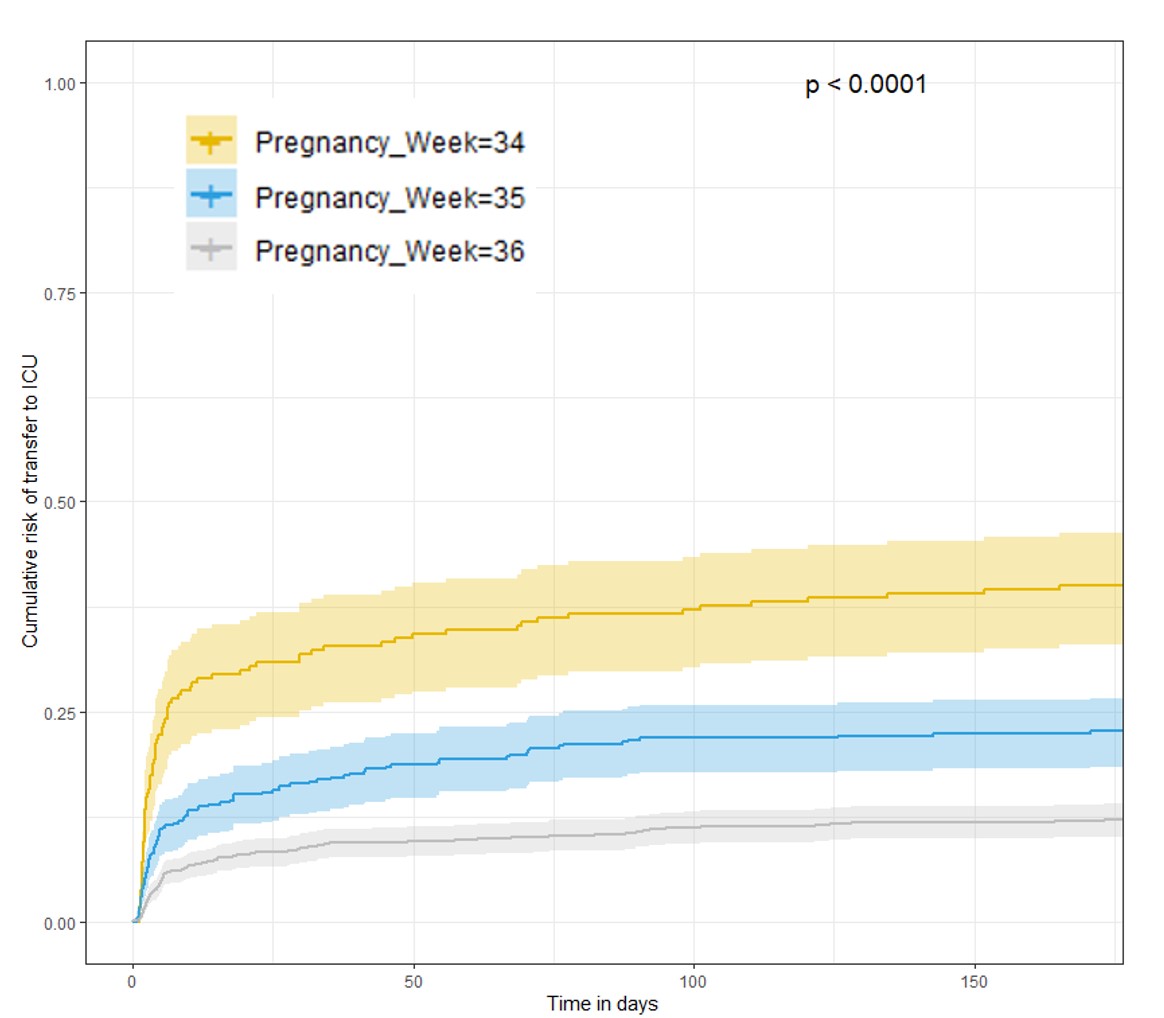
Figure 1: Neonatal intensive care unit admission rate of late preterm infants by gestational age.