Neonatal/Infant Resuscitation 1
Session: Neonatal/Infant Resuscitation 1
285 - Relevance of leak during neonatal stabilization: A bench study finding low resistance resuscitation devices provide more stable CPAP
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 285.6318
Viktoria Gruber, Medical University Graz, Department of Paediatrics and Adolescent Medicine, Division of Neonatology, Graz, Austria, Sydney, New South Wales, Australia; Stephanie Morakeas, University of Sydney and Westmead Hospital, Sydney, New South Wales, Australia; Murray Hinder, The University of Sydney, Westmead Children's Hospital, Leura, New South Wales, Australia; Thomas Drevhammar, Karolinska Institutet, Stockholm, Stockholms Lan, Sweden; Mithilesh Dronavalli, Western Sydney University, Sydney, New South Wales, Australia; Mark B. Tracy, Westmead Hosptial NICU and the University of Sydney, Sydney, New South Wales, Australia

Viktoria Gruber, MD (she/her/hers)
Fellow
Medical University Graz
Sydney, New South Wales, Australia
Presenting Author(s)
Background: Leak impacts resuscitation device performance and has been extensively studied for positive pressure ventilation but less is known with CPAP support during spontaneous breathing. Resuscitation devices used for CPAP delivery can have different imposed resistances impacting pressure stability and their performance in the presence of leak.
Objective: Compare CPAP performance of two resuscitation devices with differing imposed resistance (R) (Neopuff (NP) T-Piece high R and rPAP low R). Sequentially greater system leaks were induced to a neonatal lung model simulating a spontaneously breathing term infant at birth with respiratory distress.
Design/Methods: Devices were tested on the lung model (Compliance 1.0 ml/cmH2O) with no leak (L0) and three incremental leak levels (L1,2,3). Leaks were continuous via differing-length side port tubes to the atmosphere. Data were collected at CPAP levels of 5,7 and 9 cmH2O. Measured parameters included mean airway pressure, fluctuation in mean pressure (∆ P), tidal volume (VT) and leak flow.
Results: 2437 breaths were analyzed. Measured PEEP cmH2O at highest leak (L3) set PEEP of 9 was 2.6 vs 7 cmH2O (NP, rPAP) and at set PEEP 5, 1.8 vs 4.1 cmH2O (NP, rPAP).
∆P at set of PEEP 9 decreased from 11.3 L0 to 5 cmH2O L3 for NP and increased from 1.9 L0 to 3.5 cmH2O L3 for rPAP.
VT was lower with NP compared to spontaneous breathing without device because of the imposed resistance and increased with higher leaks, 18 L0 vs 21.9 ml L3 and led to a small VT drop with rPAP, 23.2 vs 22.3 ml L0 vs L3, both at set PEEP 9. Mean leak flow was 0.7 vs 0.8 L/min Neopuff vs rPAP (L1, PEEP 5) and 4.4 vs 8.2 L/min Neopuff vs rPAP (L3, PEEP 9).
Conclusion(s): The low-resistance device (rPAP) maintained CPAP closer to the set value at all leak levels than the high-resistance device (NP). Higher leak flows were seen with low resistance device to maintain distending pressure at high leaks. Provision of stable CPAP is important in newborn stabilization where both face mask leak, and clinical assessment skill levels can be variable.
Figure 1
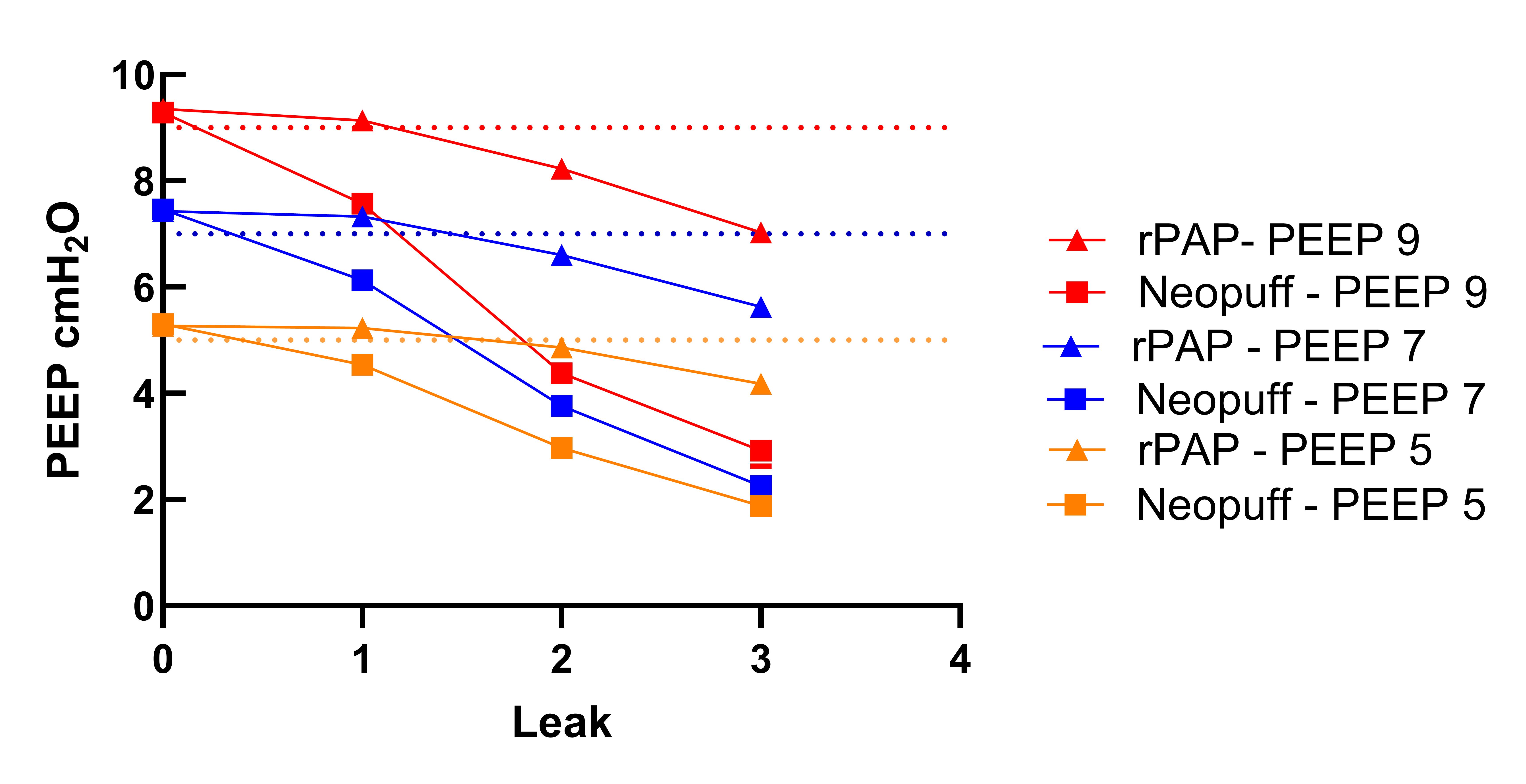 PEEP pressure of Neopuff and rPAP at different leak levels (1,2,3) for set PEEP 5,7,9 cmH2O
PEEP pressure of Neopuff and rPAP at different leak levels (1,2,3) for set PEEP 5,7,9 cmH2OFigure 2
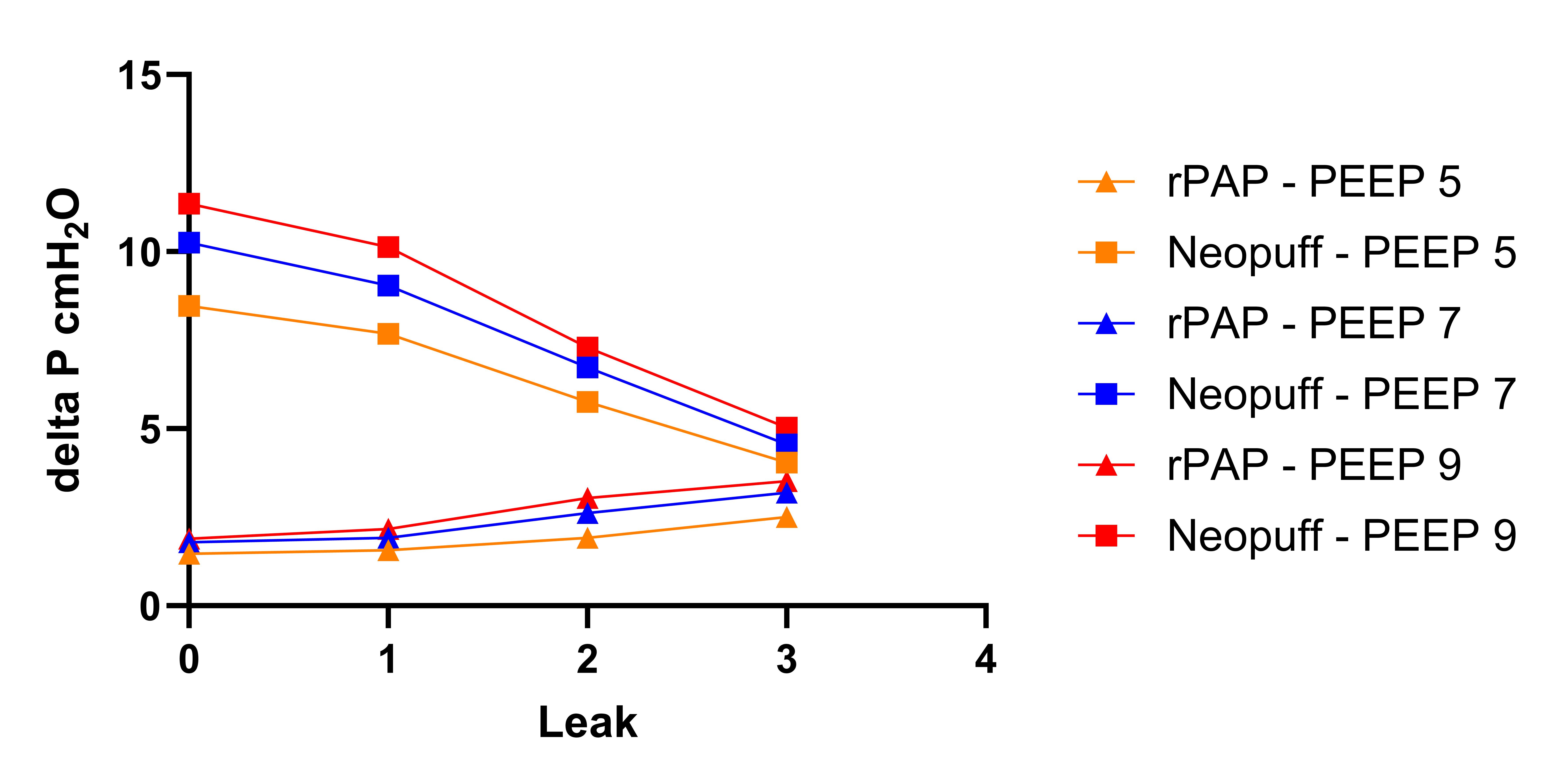 Pressure swings (∆ P) for Neopuff and rPAP at different leak levels and set PEEP 5,7,9 cmH2O
Pressure swings (∆ P) for Neopuff and rPAP at different leak levels and set PEEP 5,7,9 cmH2OFigure 3
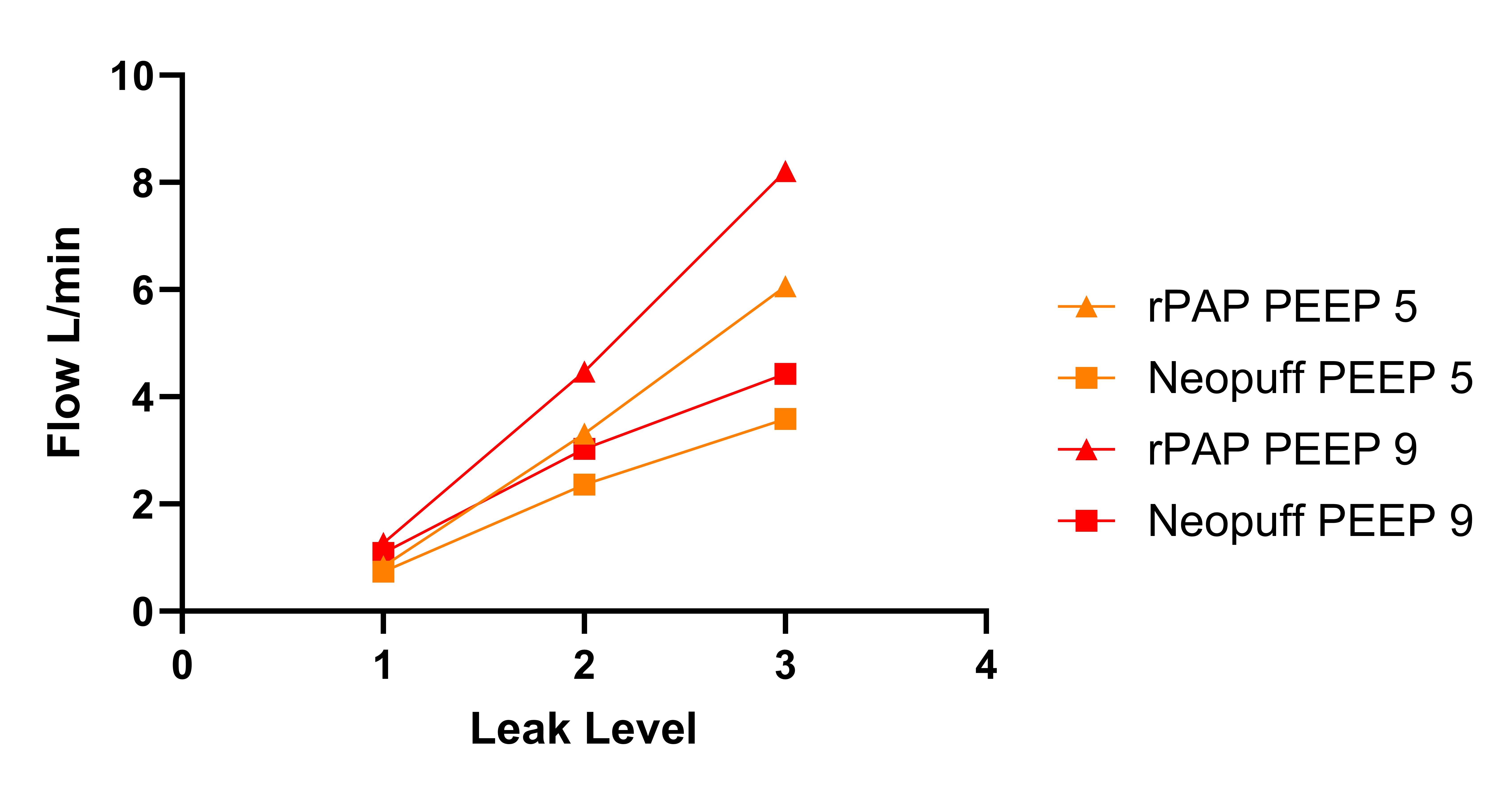 Leak flow for Neopuff and rPAP at induced leak levels (1,2,3) for PEEP 5,9 cmH2O
Leak flow for Neopuff and rPAP at induced leak levels (1,2,3) for PEEP 5,9 cmH2O
