Neonatal General 3: NICU Practices
Session: Neonatal General 3: NICU Practices
551 - Evaluating the Gaps: Quality of Prenatal Counseling Documentation in Late Preterm Gestations - A Mixed Methods Study
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 551.4813
Thea DeBroux, University of Washington School of Medicine, San Diego, CA, United States; Rachel A.. Umoren, University of Washington, Seattle, WA, United States; Megan Gray, University of Washington School of Medicine, Seattle, WA, United States; Isabella Eck, University of Washington School of Medicine, Boise, ID, United States; Hannah Benjamin, University of Washington School of Medicine, Seattle Wa, WA, United States; Michelle J. Bartlett, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jasmine James, University of Washington, Seattle, WA, United States
.jpeg.jpg)
Thea DeBroux (she/her/hers)
Research Assistant
University of Washington School of Medicine
San Diego, California, United States
Presenting Author(s)
Background: Late preterm (LPT) infants are more likely to experience health complications compared to term infants and comprise 75% of premature births. Prenatal counseling provides education and emotional support to families expecting late preterm infants and helps build trust in the medical team. Adequate documentation of these prenatal counseling visits is vital for promoting high-quality, family-centered care. Resident education and updates to the prenatal counseling note template were employed with an aim to enhance prenatal counseling documentation across the University of Washington Medicine System.
Objective: To evaluate the frequency and content of prenatal consultations notes prior to late preterm deliveries to inform prenatal counseling documentation quality improvement efforts.
Design/Methods: A retrospective chart review of documented prenatal consultations offered by obstetric (OB), pediatric and family medicine (FM) providers from 34-37 weeks gestation was performed through Apr-Jun 2022 (epoch 1) and Apr-Jun 2024 (epoch 2) at a single delivery hospital with a level III NICU. Admission and prenatal counseling notes were reviewed for documented phrases indicating awareness of, or response to the patient’s perspective and concerns. Text analysis was conducted for frequency and content of six elements representing patient preferences and perspective using Linguistic Inquiry and Word Count (LIWC) software.
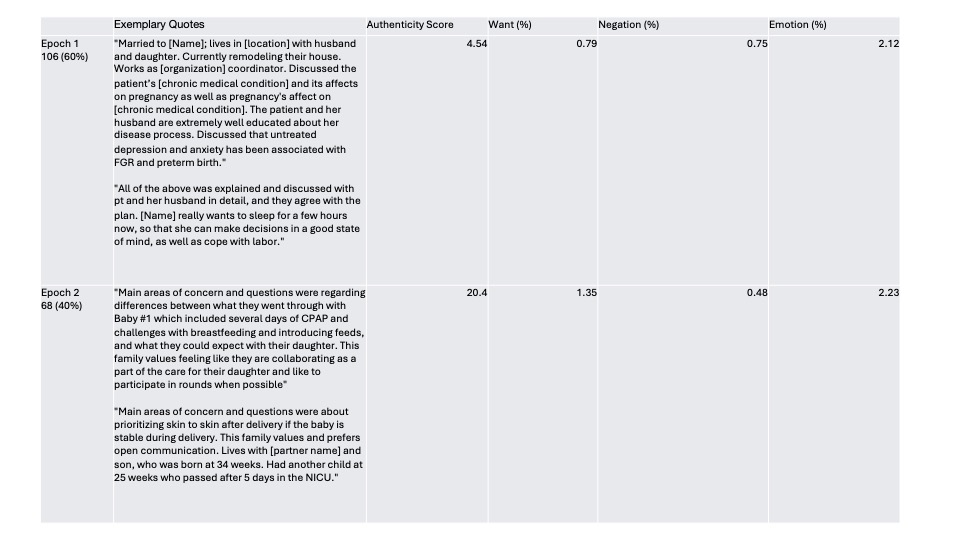
Results: Across both epochs, 174 patients presented with late preterm pregnancies (106 epoch 1 and 68 epoch 2). Median gestation at the time of admission was 35.3 weeks (IQR 34.6-36.2). Table 1. Documentation of prenatal counseling for LPT status was 32% in epoch 1 and 35% in epoch 2. Despite an increase in family-centered counseling elements in epoch 2, most notes from both epochs were still missing key components (Figure 2). Across both epochs, emotional markers were present in 2% of words, as determined by LIWC analysis. Chart review showed similar results, with 8% of notes in both epochs presenting an emotional response. Authenticity and “want” word frequencies were higher in epoch 2, suggesting increased documentation of patient preferences. Family-centered counseling elements were generally more frequently noted epoch 2, with the exception of emotional response documentation. Figure 3.
Conclusion(s): Elements of family-centered prenatal counseling documentation increased after the implementation of resident education and a new note template. However, there remain opportunities to improve prenatal counseling documentation which can further inform QI efforts to improve family-centered care.
Figure 1. Documentation of Family-Centered Prenatal Counseling Elements
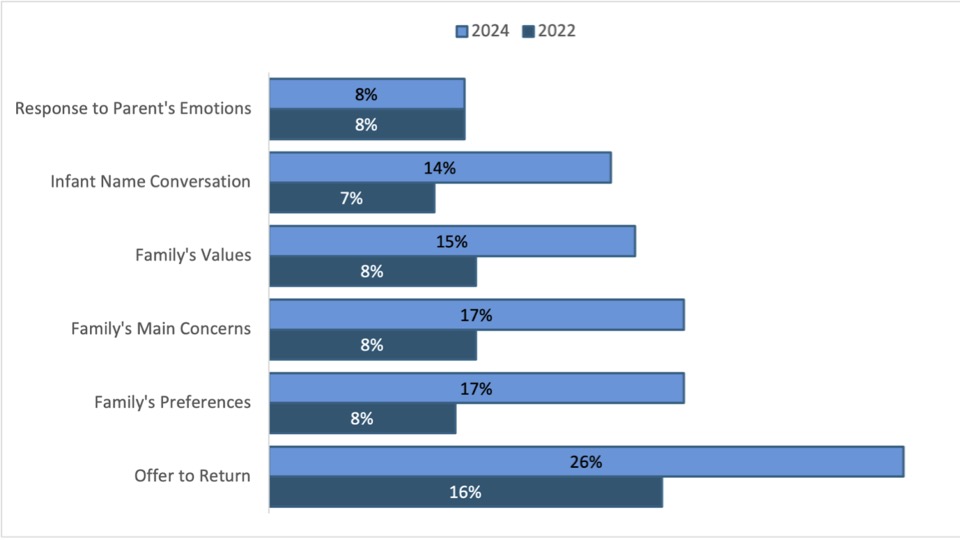
Table 1. Demographics
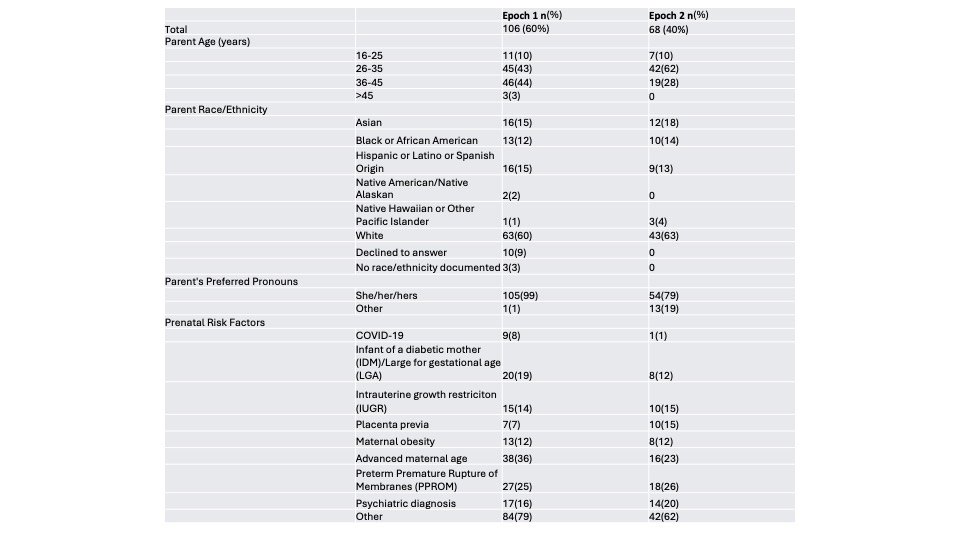
Table 2. Exemplary Quotes of Documented Notes and LIWC Analysis