Emergency Medicine 4
Session: Emergency Medicine 4
247 - How do Pediatric Emergency Medicine Fellows Learn Clinical Operations? A Needs Assessment and Current Practice Survey
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 247.5188
Katherine Ryan, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Cindy Ganis. Roskind, Columbia University Vagelos College of Physicians and Surgeons, purchase, NY, United States; Nazreen Jamal, Columbia University Vagelos College of Physicians and Surgeons, Closter, NJ, United States

Katherine Ryan, MD (she/her/hers)
Fellow Physician
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Administrative and leadership skills are critical for emergency physicians who lead multidisciplinary teams and manage operational tasks daily. Although the ACGME requirements outline key administrative competencies, many pediatric emergency medicine (PEM) fellows do not achieve full proficiency in these areas, and no standardized curriculum currently exists to teach these skills.
Objective: Our primary aim is to describe existing practices for teaching administrative, operational, and leadership topics in PEM fellowship programs. Our secondary aim is to identify specific content areas for future curricula.
Design/Methods: We conducted a cross-sectional, internet-based survey targeting PEM fellowship program directors (PDs) and current and former fellows. Using the American Academy of Pediatrics Section of Emergency Medicine’s PEM PD listserv, we identified 77 programs, including 400 second- and third-year fellows and 400 recent graduates. Separate surveys for PDs and fellows focused on the presence of operations curricula and perceived readiness for post-graduation administrative responsibilities. Data were analyzed using descriptive statistics and open-ended responses were reviewed to extract common themes.
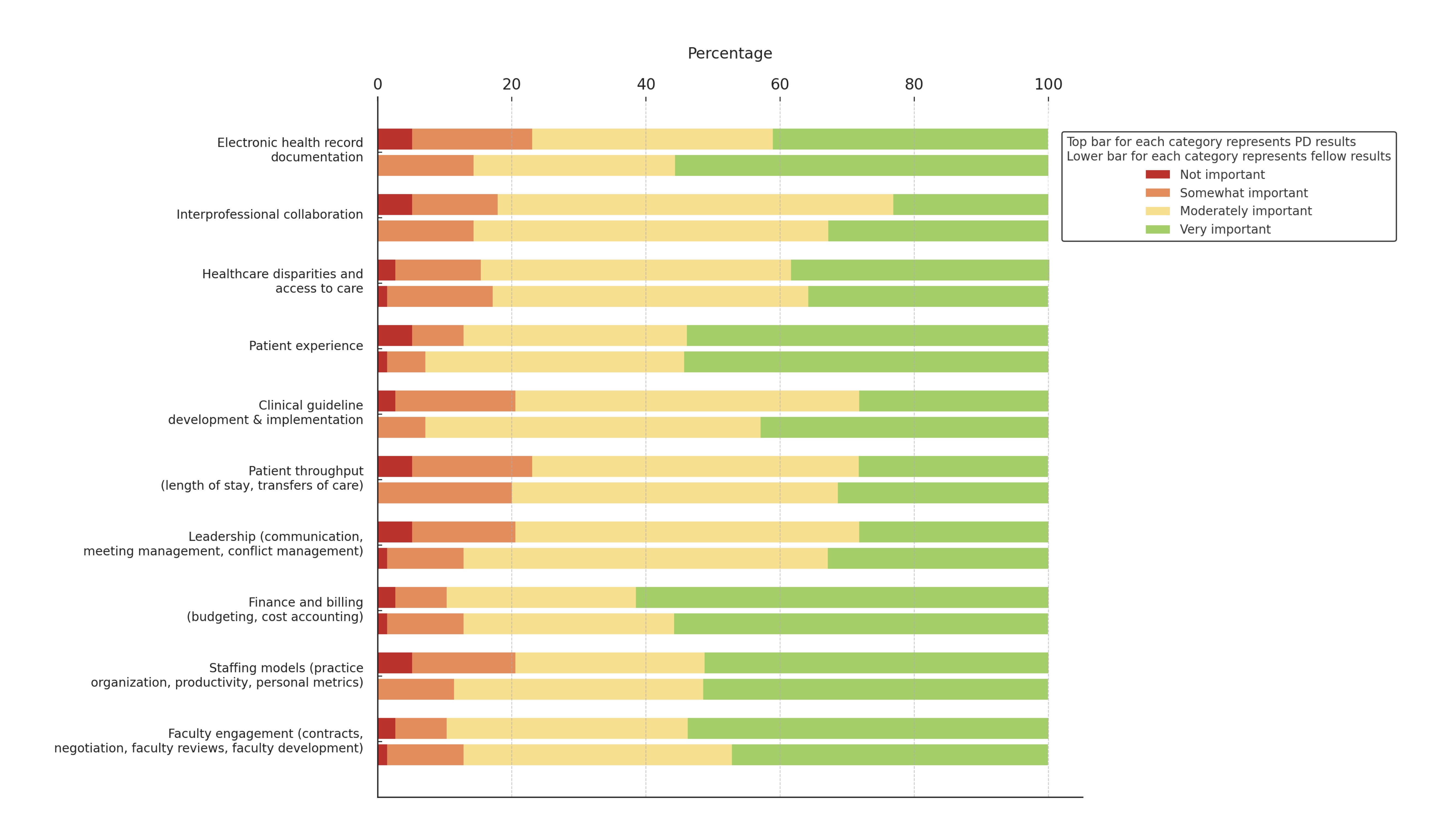
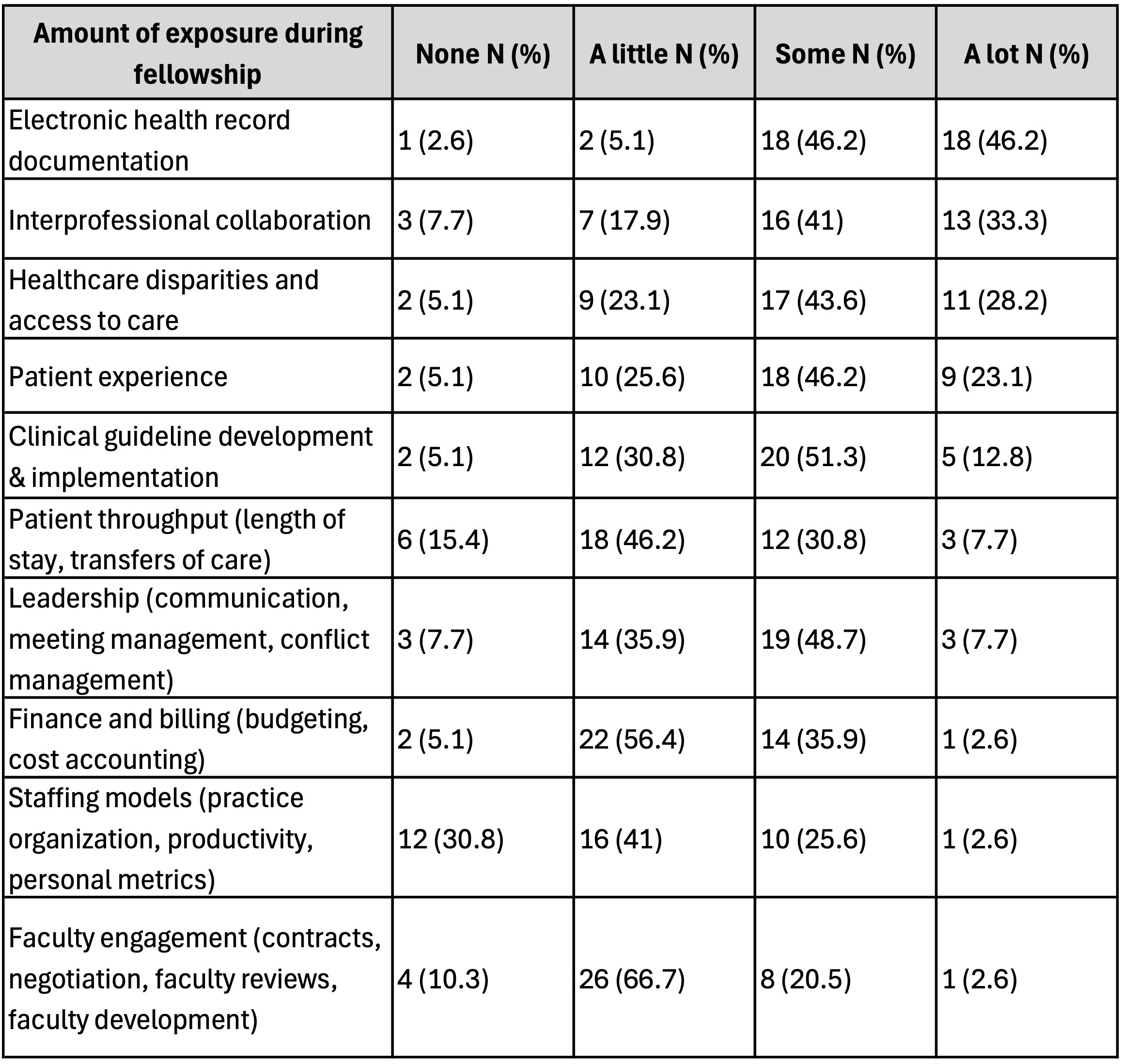
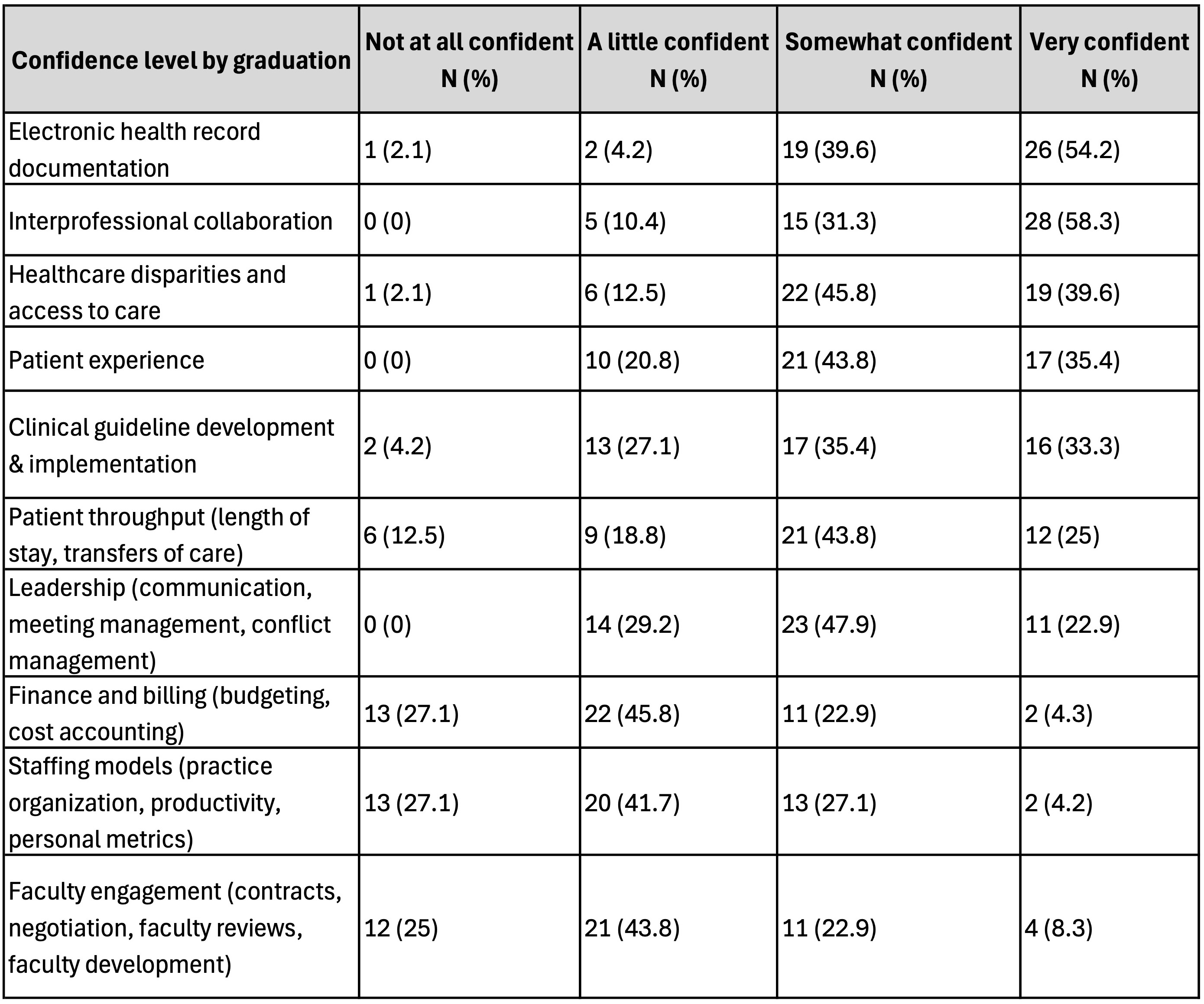
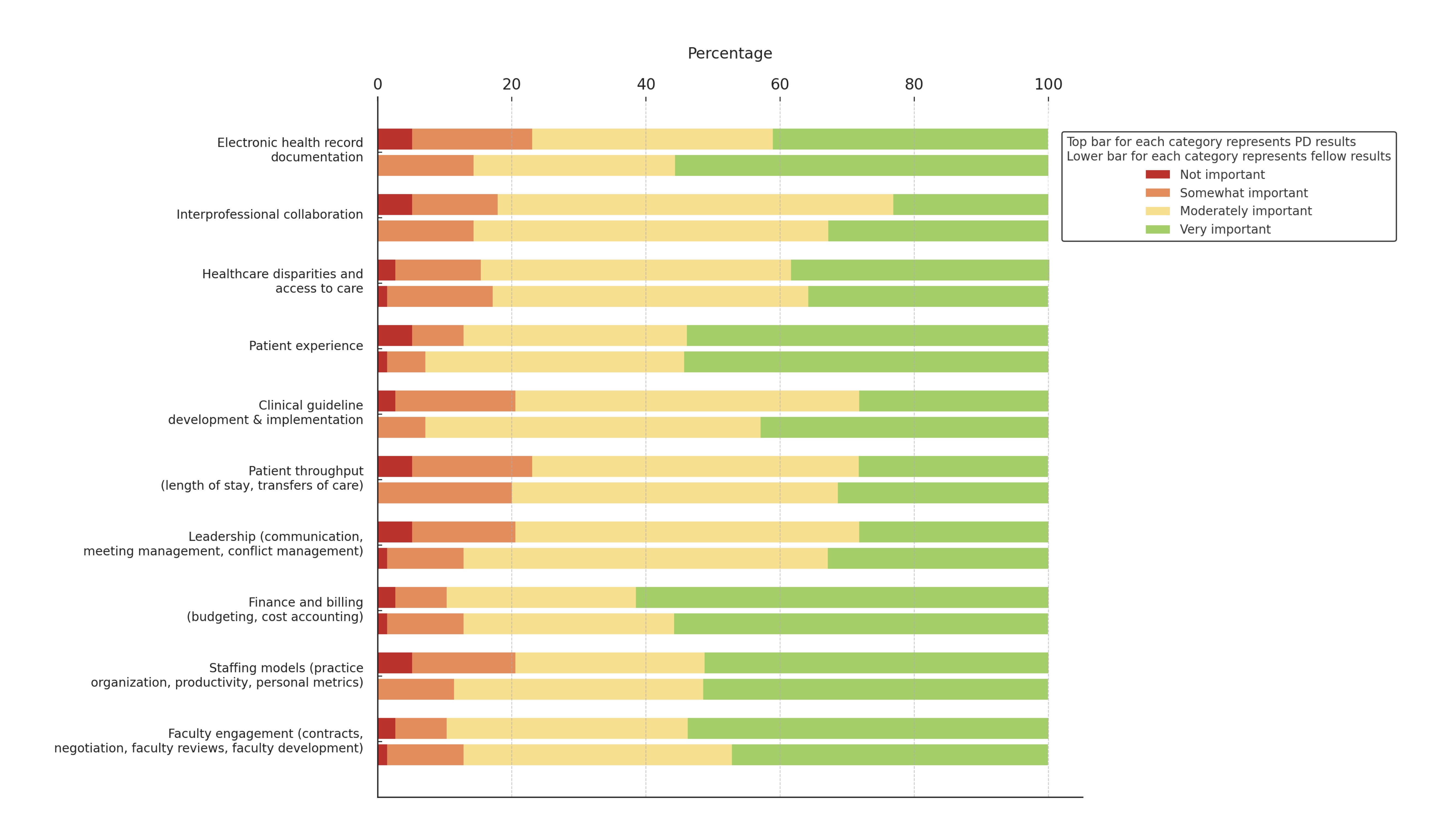
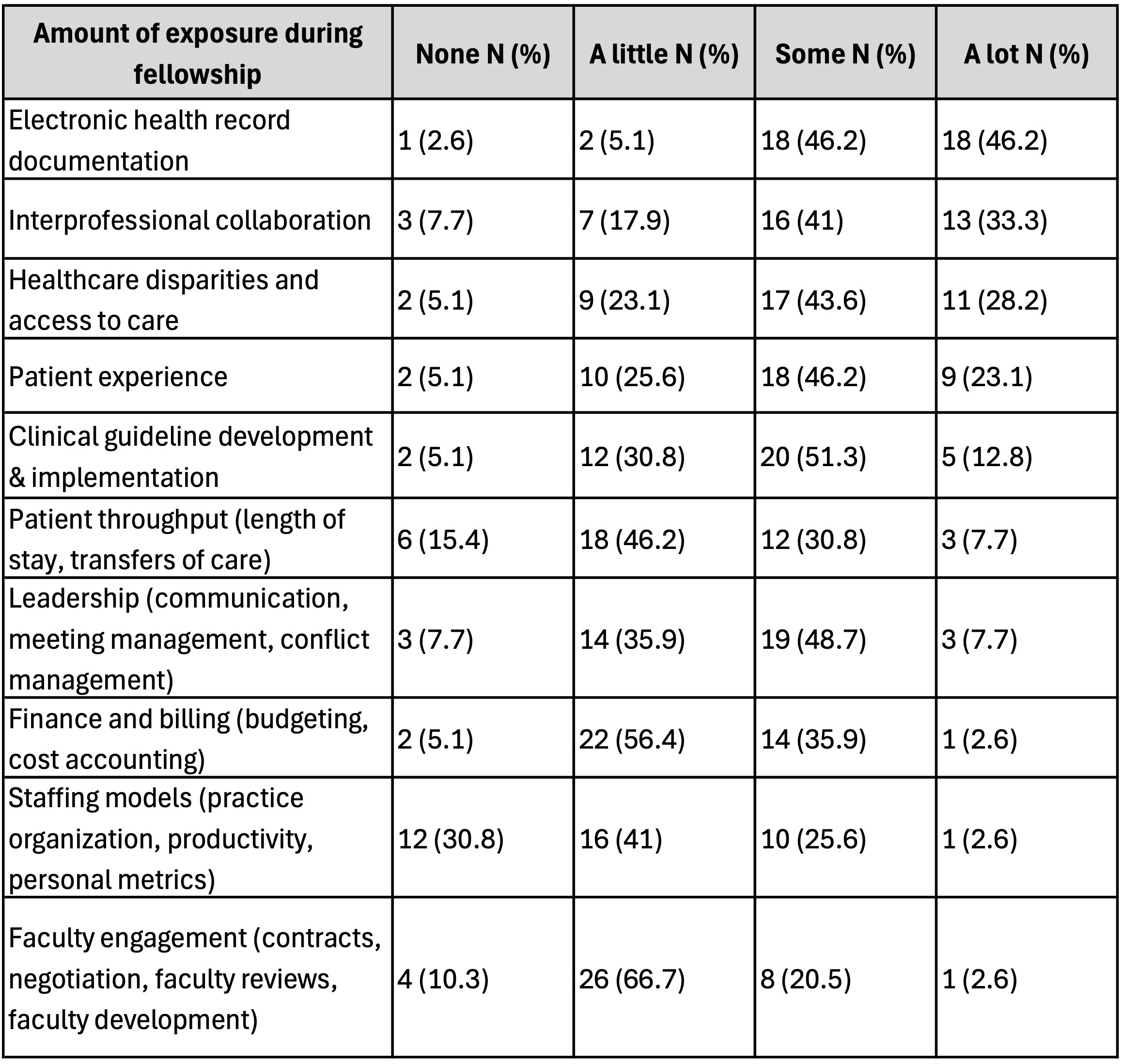
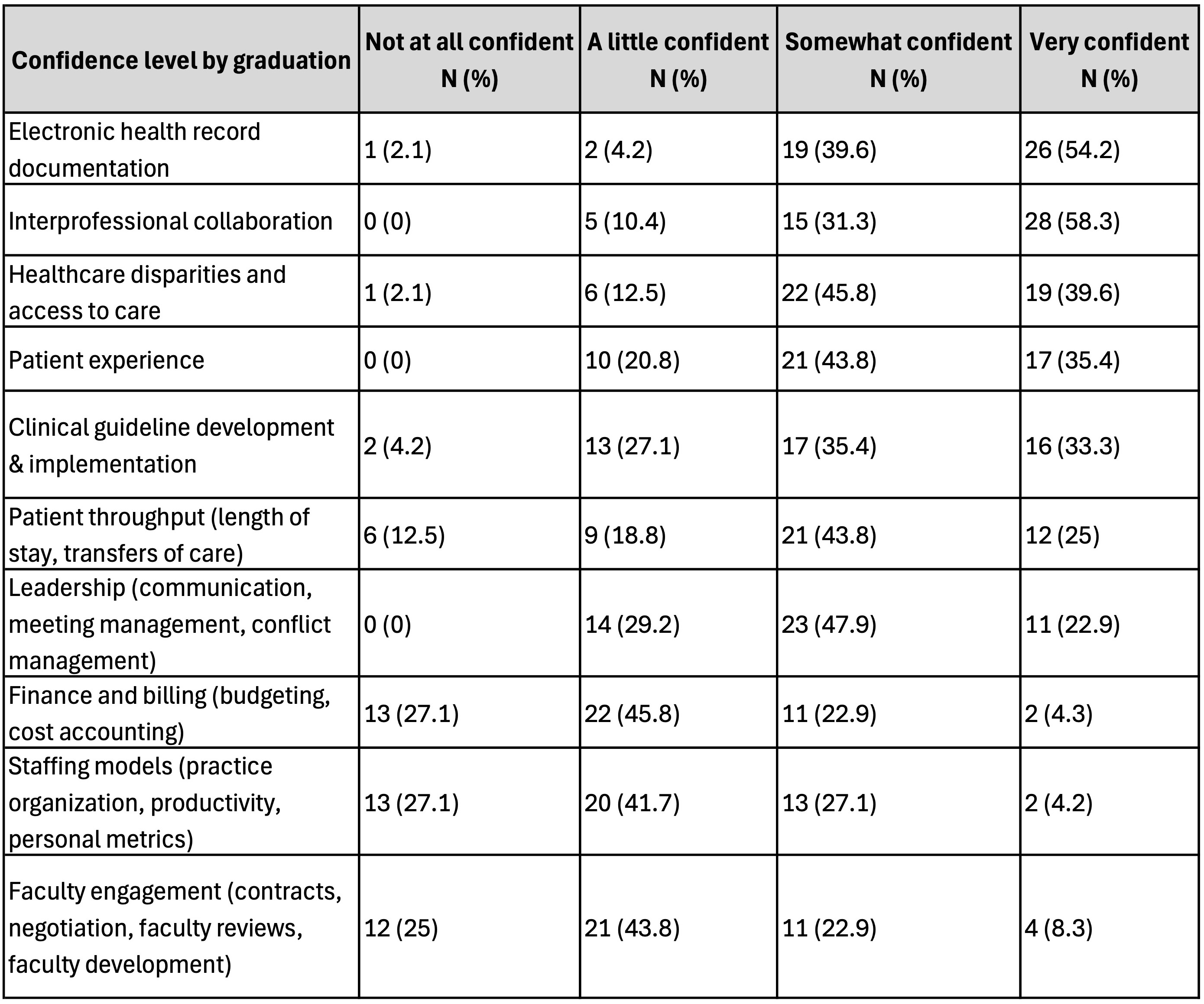
Results: Respondents included 42/77 PDs (55%) and 75/336 fellows (22%). Most PDs (81%, 34/42) and fellows (64%, 48/75) reported no formal operations curricula in their programs. 65% (22/34) of PDs without a curriculum expressed interest in adopting one, and 97% (30/31) of current fellows without exposure to a curriculum expressed interest in participating. The biggest barrier to implementation for PDs not intending to create a curriculum was lack of time (67%, 8/12). PDs reported that their fellows receive limited exposure to topics such as faculty engagement/development (77%, 30/39), staffing models (72%, 28/39), finance and billing (62%, 24/39), and patient throughput (62%, 24/39) (Table 1). Fellows and recent graduates also reported low confidence in these areas (Table 2). PDs (62%, 24/39) and fellows (56%, 39/70) identified healthcare disparities/access to care as the most important topic to include in a future curriculum (Figure 1).
Conclusion(s): This study highlights significant variability in the presence and content of operations curricula within PEM fellowship programs. Although some programs provide formal training, many fellows report a lack of confidence in administrative and operational skills, underscoring the need for a standardized curriculum to ensure PEM fellows are prepared for administrative and operational roles post-graduation.
Exposure to Key Operational Topics Among PEM Fellows as Reported by Program Directors
Confidence Levels of Fellows and Graduates in Operational Competencies
Key Topics for Inclusion in an Operations Curriculum: Program Director and Fellow Perspectives
Exposure to Key Operational Topics Among PEM Fellows as Reported by Program Directors
Confidence Levels of Fellows and Graduates in Operational Competencies
Key Topics for Inclusion in an Operations Curriculum: Program Director and Fellow Perspectives