Emergency Medicine 6
Session: Emergency Medicine 6
280 - Epidemiology of Potential Missed Diagnosis of Pediatric Central Nervous System Infections in the Emergency Department
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 280.5057
Kaileen Jafari, University of Washington School of Medicine, Seattle, WA, United States; Yasaman Fatemi, University of Washington School of Medicine, Seattle, WA, United States; Apeksha Gupta, SCH, BELLEVUE, WA, United States; Eileen Klein, Seattle Children's, Seattle, WA, United States; Prashant Mahajan, University of Michigan Medical School, Troy, MI, United States
- KJ
Kaileen Jafari, MD
Assistant Professor
University of Washington School of Medicine
Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Pediatric central nervous system infections (CNSi), including meningitis, craniospinal abscess, and encephalitis, can lead to significant morbidity especially if treatment is delayed. However, early diagnosis of CNSi challenging due to non-specific symptoms particularly in young children.
Objective: To assess the frequency and predictors of potentially missed diagnoses of pediatric CNSi in emergency department (ED) visits and evaluate whether potential missed diagnoses were associated with to severe neurologic complications.
Design/Methods: Cross-sectional analysis of the 2018-2019 Healthcare Cost and Utilization Project State ED and Inpatient Datasets from five states. Inpatient admissions for patients < 18 years with CNSi were included, those without linkage variables or with pre-existing intracranial hardware were excluded( Figure 1). Potential missed diagnosis was defined as a 30-day antecedent ED treat-and-release visit with a high-risk ED diagnosis defined using Symptom-Disease Pair Analysis of Diagnostic Error methodology(Table 1). Severe neurologic complications was defined as any of the following diagnoses (stroke, intracranial bleed, cerebral edema, ventricular shunt/ventriculostomy), procedures( spinal/intracranial decompression procedures) or death/discharge to rehab. Descriptive statistics, chi-square/ANOVA, and Kruskal-Wallis tests were utilized to compare groups; mixed-effects logistic regression was used to identify predictors of potential missed diagnosis and neurologic complications.
Results: Out of 2,686 CNSi cases, 342 (12.7%) had a potential missed diagnosis. Fever (n=167, 35.9%), headache(n=126, 27.1%), and vomiting(n=86,18.5%) were the most frequent ED diagnoses observed at preceding ED visits(Table 1). In multivariable analysis, predictors of potential missed diagnosis included age over 90 days (OR 4.64, 95%CI 3.22-6.70), Black (OR 1.86, 95%CI 1.35-2.57) or Asian race (OR 1.75, 95%CI 1.09-2.81). In the subset of bacterial CNSi cases, potential missed diagnoses were associated with a higher risk of neurologic complications (OR 2.09 95%CI 1.19-3.65) after adjusting for age, chronic conditions, revisit interval, and bacterial CNSi subtype( Table 2). No such association was observed in the viral/other CNSi subset.
Conclusion(s): Age >90 days and Black or Asian race/ethnicity were associated with potential missed diagnosis of CNSi. In bacterial CNSi, potential missed diagnosis was associated with increased risk of severe neurologic complications. Future research on diagnostic improvement in bacterial CNSi is needed, particularly in children beyond the neonatal period.
Figure 1. Sample selection methodology for identification of CNSi cases and classification of same day and potential missed diagnosis
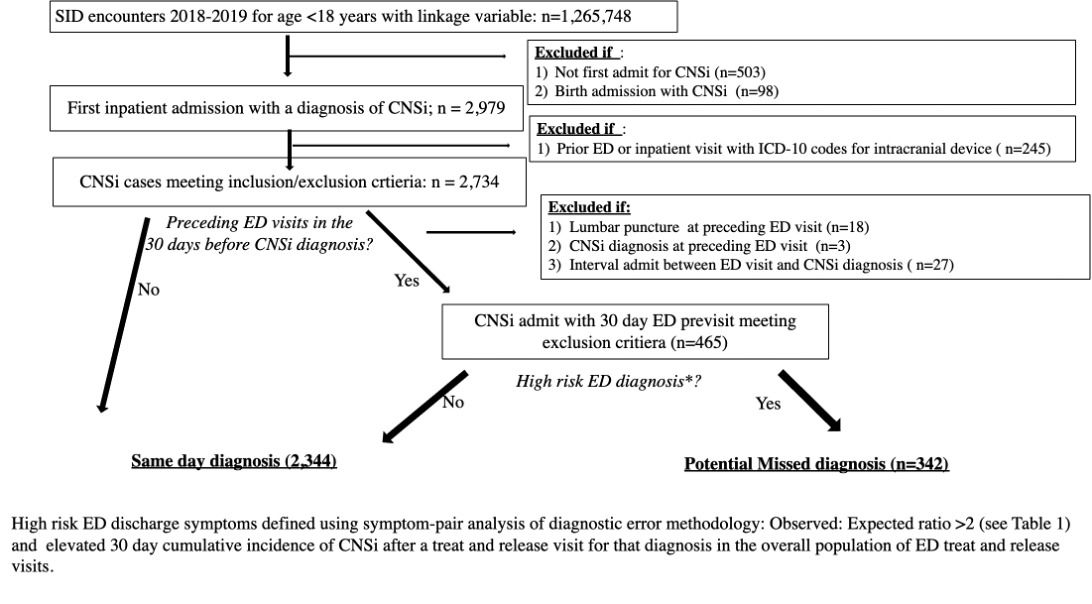
Table 1. Observed to expected ratios of "high risk" ED diagnoses at ED visits preceding CNSi diagnosis
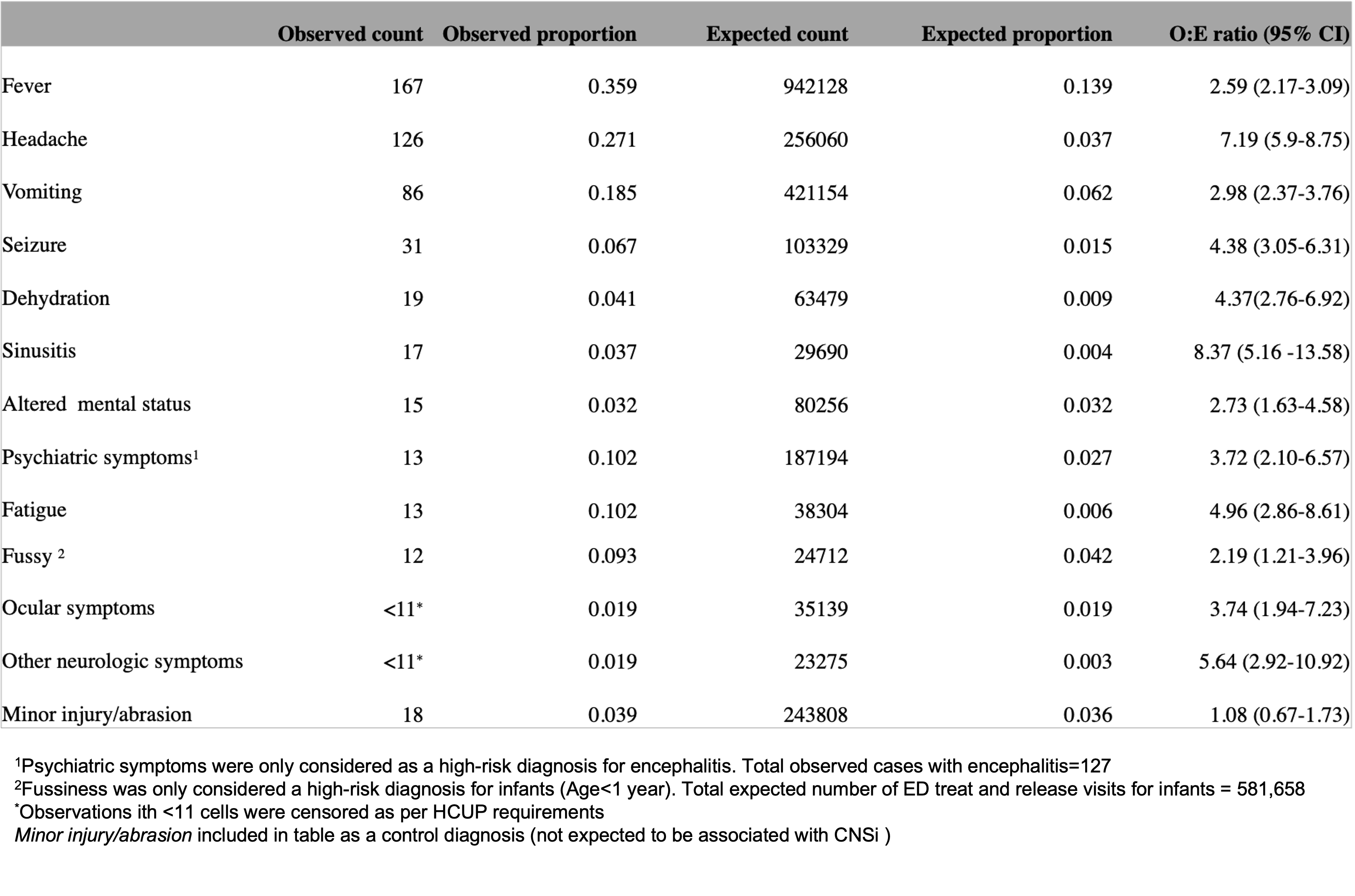 Observed:Expected ratio is the ratio of observed proportion (proportion of diagnosis in ED visits preceding CNSi diagnosis) to expected proportion (proportion of that diagnosis in overall population of ED treat and release visits in the dataset).
Observed:Expected ratio is the ratio of observed proportion (proportion of diagnosis in ED visits preceding CNSi diagnosis) to expected proportion (proportion of that diagnosis in overall population of ED treat and release visits in the dataset). Table 2. . Predictors of severe neurologic complications in CNSi using mixed effects logistic regression in subets of bacterial CNSi(A) and viral/other CNSi cases(B)
.png) A) Bacterial CNSi includes bacterial meningitis and craniospinal abscess and B) Viral or Other CNSi includes viral or other (fungal, atypical bacterial or unspecified) meningitis or encephalitis
A) Bacterial CNSi includes bacterial meningitis and craniospinal abscess and B) Viral or Other CNSi includes viral or other (fungal, atypical bacterial or unspecified) meningitis or encephalitis
