Emergency Medicine 6
Session: Emergency Medicine 6
277 - Duration of Emergency Department Diagnostic Delay is Associated with Acute Complications of Pediatric Deep-Seated Bacterial Infections
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 277.5060
Kaileen Jafari, University of Washington School of Medicine, Seattle, WA, United States; Yasaman Fatemi, University of Washington School of Medicine, Seattle, WA, United States; Apeksha Gupta, SCH, BELLEVUE, WA, United States; Eileen Klein, Seattle Children's, Seattle, WA, United States; Prashant Mahajan, University of Michigan Medical School, Troy, MI, United States
- KJ
Kaileen Jafari, MD
Assistant Professor
University of Washington School of Medicine
Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Deep-seated bacterial infections (DSBi), defined as infections deeper that skin/superficial anatomical spaces including meningitis and craniospinal abscess; thoracic empyema; osteoarticular and deep neck space infections are infrequent in children and challenging to diagnose in a timely and accurate manner. The association and duration between prior emergency department (ED) visits and the eventual ED and/or inpatient diagnosis of select DSBi and its associated complications is under explored.
Objective: To determine if duration of ED diagnostic delay is associated with risk of acute complications of pediatric DSBi.
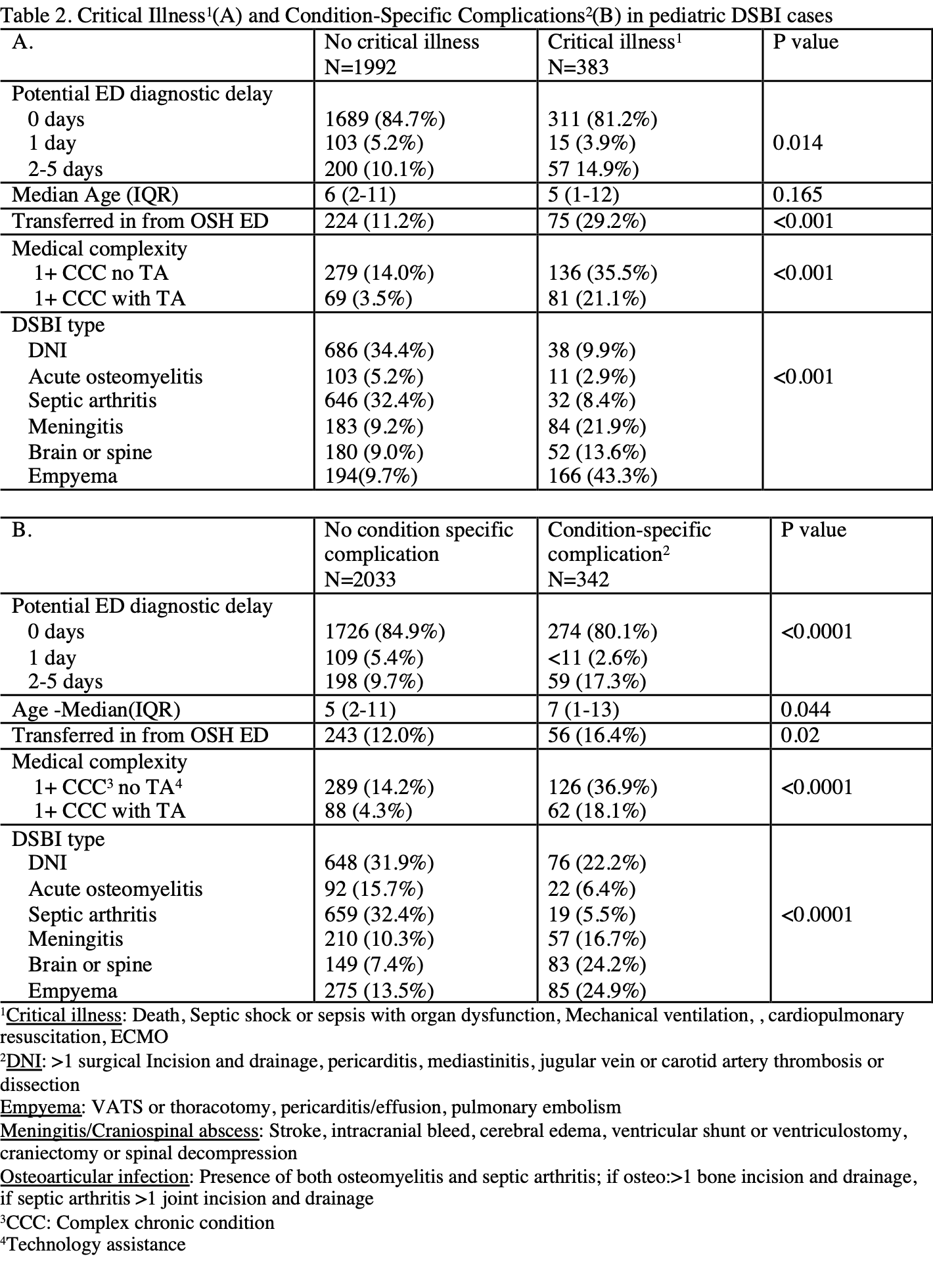
Design/Methods: Cross-sectional analysis of 2018-2019 HCUP State ED and Inpatient Datasets from 5 states. Hospital admissions for DSBi for patients < 18 years were included (Figure 1). Potential delayed diagnosis, defined as an ED treat-and-release visit in the 1-5 days prior to DSBI diagnosis, was grouped into 1-day and 2-5 day delayed diagnosis based upon the ED visit to return visit interval. The primary outcome was critical illness during DSBi admission and secondary outcome was any acute condition-specific complications during the DSBi admission (Table 2). Descriptive statistics were used to compare patient characteristics and outcomes (Table 1, 2); chi-square and Kruskal-Wallis were used to compare categorical and continuous variables, respectively. Mixed effects logistic regression was used to determine predictors associated with critical illness or condition-specific complications.
Results: Of 2,375 inpatient admissions for DSBi; 19.4% had a potential delayed diagnosis; 5.0% with a 1 day delay and 14.4% with a 2-5 day delay. Black, Hispanic patients and those in the lowest income quartile were more likely to have a potential delayed diagnosis of 2-5 days vs. 1 day or no delay (Black 20% vs. 14% vs. 17%; Hispanic 33% vs. 25% vs. 29%, p= 0.036; lower two income quartiles( 66% vs. 57% vs. 59%, p=0.03). In the regression models, after adjusting for complex chronic conditions, DSBi type, age, and transfer status, patients with potential diagnostic delay of 2-5 days had an increased risk of critical illness aOR 1.62 (1.12-2.36) and condition specific complications aOR 2.10 (1.48-2.96) compared to the no diagnostic delay group, while those with a return visit of 1 day had no difference in risk of critical illness (aOR 1.05,95% CI 0.57-1.94) or condition-specific complications (aOR 0.62, 95%CI 0.30-1.27).
Conclusion(s): Longer duration of potential ED diagnostic delay is associated with increased risk of critical illness and condition-specific complications of DSBi in children.
Figure 1. Sample Selection Methodology
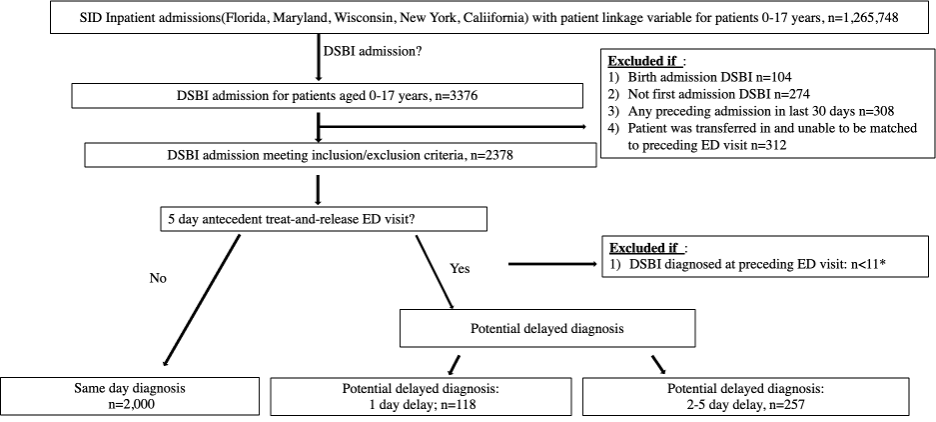
Table 1. Baseline characteristics of DSBI cases
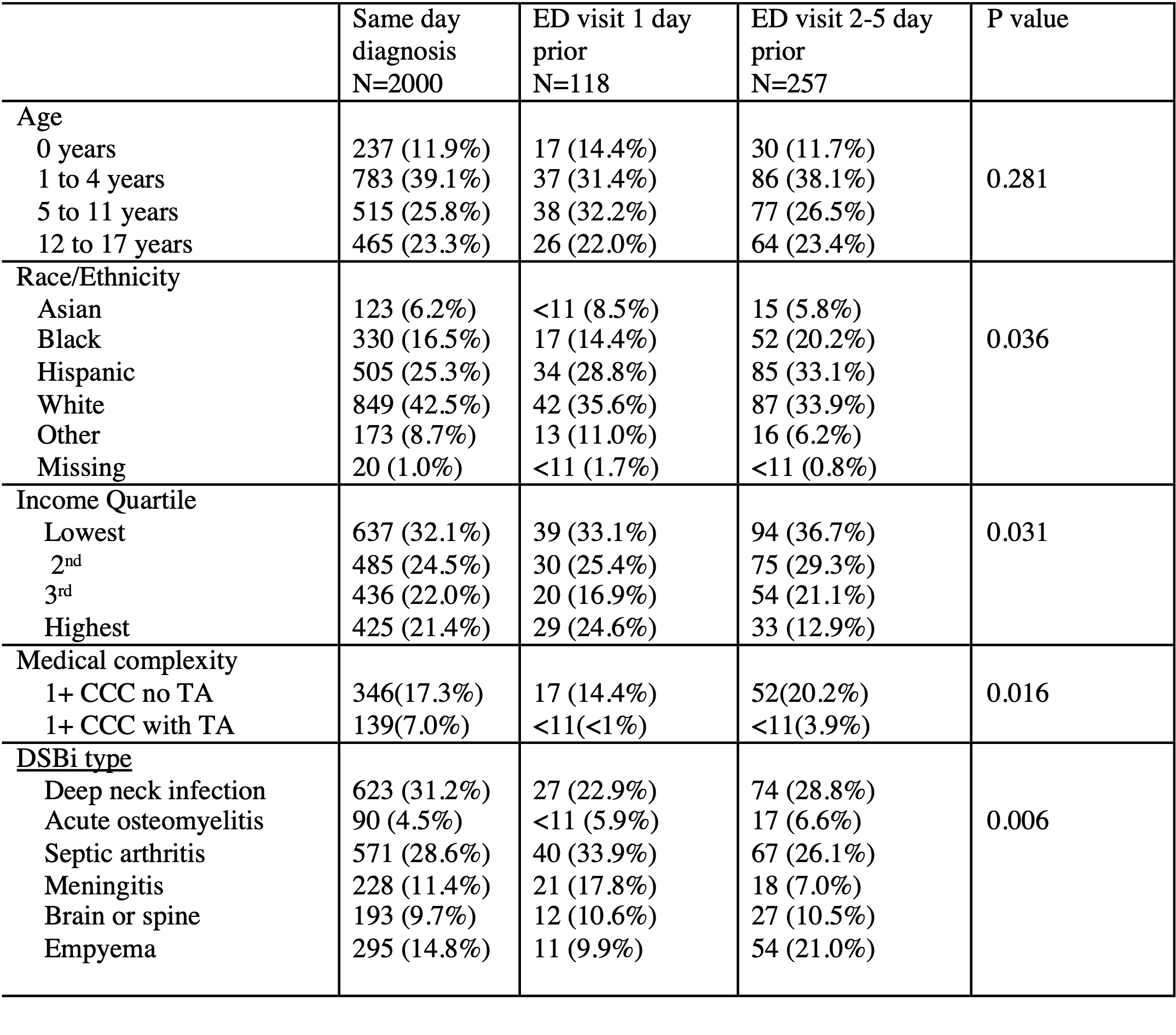
Table 2. Critical Illness(A) and Condition-Specific Complications(B) in pediatric DSBI cases