Neonatal General 1: Respiratory, BPD
Session: Neonatal General 1: Respiratory, BPD
273 - Predicting Extubation Success in Premature Infants
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 273.6273
Victoria M. Scarpelli, Cohen Children's Medical Center, Mineola, NY, United States; Stephanie Galanti, Cohen Children's Medical Center, New Hyde Park, NY, United States; Iels Aan Jibu, Feinstein Institutes for Medical Research, Hicksville, NY, United States; Alla Zaytseva, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New Hyde Park, NY, United States; Dalibor Kurepa, Northwell - Cohen Children's Medical Center, Jericho, NY, United States; Barry Weinberger, Cohen Children's Medical Center, New Hyde Park, NY, United States

Victoria M. Scarpelli, MD MPH (she/her/hers)
Fellow, Neonatal Perinatal Medicine
Cohen Children's Medical Center
Mineola, New York, United States
Presenting Author(s)
Background: Invasive mechanical ventilation is often required for extremely preterm infants but can contribute to morbidity. Objective metrics are used for assessing extubation readiness in older children and adults. However, tools that are currently available for predicting extubation success in preterm infants include only variables that are already routinely used in decision-making at the bedside, and they have not been widely adopted. In our NICU, the decision to extubate has been based on clinical judgment.
Objective: Our objectives are to identify additional predictors for extubation success and to build a predictive model that assists clinicians in determining extubation readiness for preterm infants.
Design/Methods: We conducted a retrospective chart review of demographic and medical variables preceding 320 extubation attempts for infants ≤ 30 weeks gestation or ≤ 1250 grams at birth requiring invasive mechanical ventilation for > 24 hours and extubated at < 60 days of age between January 2017 and January 2023. The primary outcome was remaining extubated for at least 24 hours. Data preprocessing was started by addressing missing data through multiple imputation by chained equations (MICE). After the dataset was scaled, it was split 80:20 into training and test datasets. All variables were evaluated using a univariate mixed effects logistic regression. Class imbalance in the training dataset was corrected using the synthetic minority over-sampling technique (SMOTE). Based on the results of the logistic regression, a predictive model was built using an elastic net regularization with 10-fold cross-validation.
Results: Of 320 extubation attempts, 272 (85%) were successful. There were 84 variables considered, of which nine were statistically significant as standalone predictors of extubation success in a mixed-effects model and were retained in the final model: gestational age at birth (GA), corrected gestational age at time of extubation (CGA), completed a postnatal steroid course, birthweight (BW), weight at extubation, mean airway pressure 24 hours prior to extubation (MAP), respiratory severity score (RSS), pH prior to extubation, and volume of enteral feeds per kilogram on day of extubation (Table 1). Performance metrics were a total accuracy of 79%, a sensitivity of 81%, a specificity of 66%, a positive predictive value of 93%, and a negative predictive value of 37%.
Conclusion(s): A model that includes elements that are not routinely considered, such as the volume of enteral feeds on the day of extubation and MAP 24 hours before extubation, can improve the prediction of extubation success.
Table 1. Predictors of extubation success
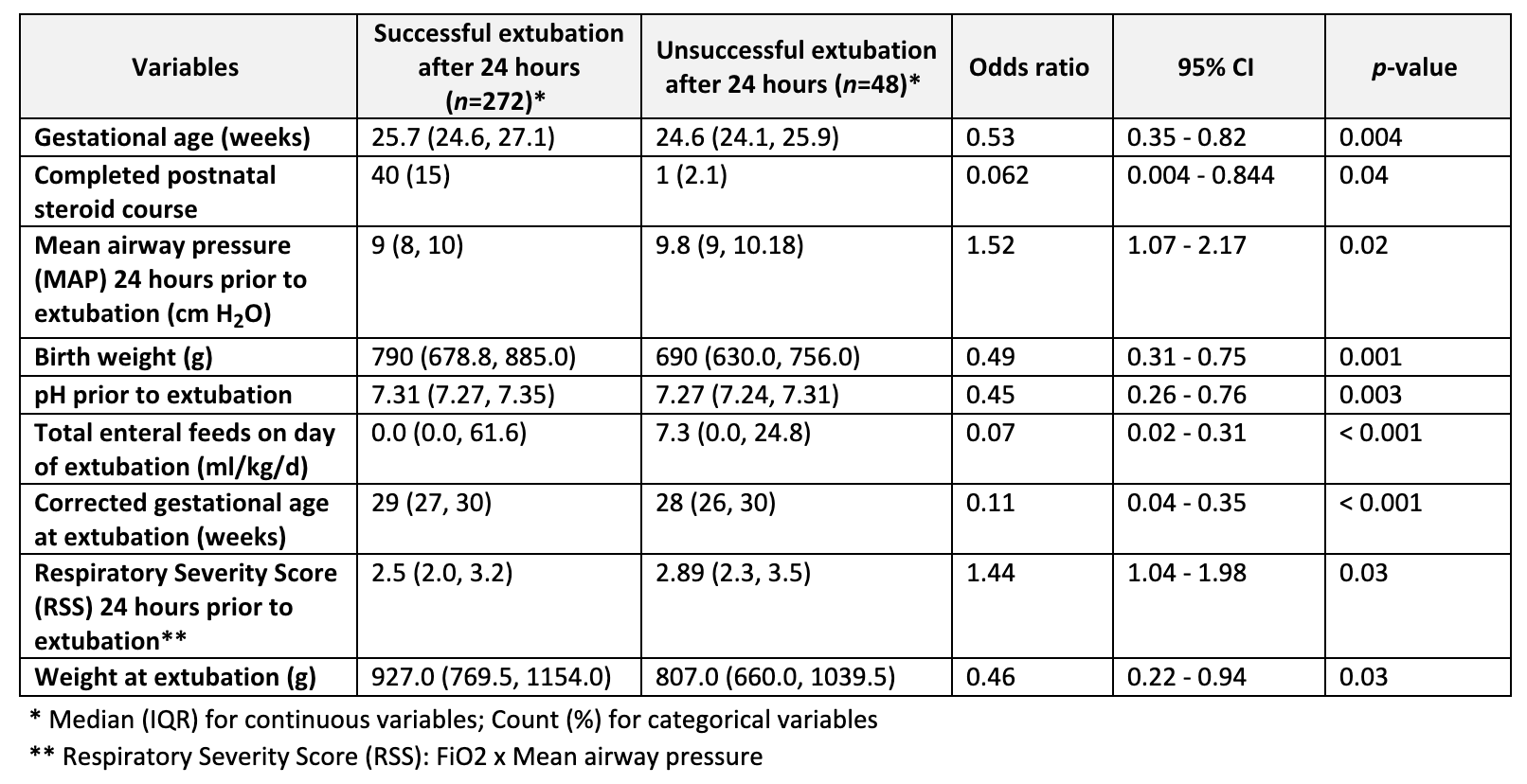 Nine variables were statistically significant as standalone predictors of extubation success in a mixed-effects logistic regression and were retained in the predictive model. Characteristics summarized with odds ratios and 95% confidence intervals.
Nine variables were statistically significant as standalone predictors of extubation success in a mixed-effects logistic regression and were retained in the predictive model. Characteristics summarized with odds ratios and 95% confidence intervals.
