Neonatal Pulmonology - Clinical 2: BPD: Incidence, Treatment, Outcomes
Session: Neonatal Pulmonology - Clinical 2: BPD: Incidence, Treatment, Outcomes
254 - Home oxygen therapy for bronchopulmonary dysplasia in Japan: A questionnaire survey
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 254.5241
Ryo Ogawa, Nagano Children's Hospital, azumino, Nagano, Japan; Masaki Hasebe, Nagano Children's Hospital, Azumino, Nagano, Japan; Tomohiko Nakamura, Nagano Children's Hospital, Azumino, Nagano, Japan; Fumihiko Namba, Saitama Medical Center, Saitama Medical University, Kawagoe, Saitama, Japan
- RO
Ryo Ogawa, MD, PhD (he/him/his)
Vice Director
Nagano Children's Hospital
azumino, Nagano, Japan
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) in preterm infants exhibits constant incidence despite neonatal care advancements. Consequently, the use of home oxygen therapy (HOT) has become a crucial component in the post-discharge management of these infants. However, guidelines for HOT introduction and management differ across countries due to insufficient evidence, and Japan lacks clear, standardized guidelines.
Objective: This study aimed to determine differences among facilities in Japan in terms of HOT introduction and management for BPD.
Design/Methods: A questionnaire survey was conducted at 112 perinatal medical centers in Japan between September 2023 and October 2023.
Results: The response rate was 91.1% (102/112). All the facilities utilized percutaneous oxygen saturation (SpO2) as a criterion for HOT initiation. The most predominant SpO2 threshold was 95% (37%), with all facilities using values between 90% and 95%; 17% demonstrating no specific reference value. Only 35% of the facilities had established standards for the duration and frequency of sub-threshold SpO2 levels. Of facilities with established criteria, 11% introduced HOT when SpO2 was below the threshold for ≥10% of the time. Pulmonary hypertension (PH) assessment was routinely performed in 83% of the facilities, mostly by neonatologists using ultrasound. However, only 30% of the facilities consistently conducted PH assessments after discharge. Pulse oximetry monitoring at home was routinely introduced in 84% of the facilities, primarily to guide HOT discontinuation (95%) and detect worsening respiratory status (90%). Of the facilities, 66% used a SpO2 threshold of ≥95% for discontinuation, but 69% lacked criteria for the duration and frequency of values below this threshold. Additionally, 67% of the facilities relied on family reports of SpO2 levels, whereas most facilities did not analyze the oximeter data. Of the facilities, only 14% analyzed the data, and only 4% admitted patients for further testing.
Conclusion(s): The study demonstrated significant variations in both the criteria for introducing HOT and its management among perinatal medical centers in Japan. These differences, along with the lack of established criteria in some facilities, underscore the pressing need for unified, evidence-based international guidelines for HOT in patients with BPD.
The SpO2 threshold for initiating HOT and the criteria for the duration and frequency of sub-threshold SpO2 levels.
.jpg) The most predominant SpO2 threshold was 95% (37%), with all facilities using values between 90% and 95%. Only 35% of the facilities had established standards for the duration and frequency of sub-threshold SpO2 levels.
The most predominant SpO2 threshold was 95% (37%), with all facilities using values between 90% and 95%. Only 35% of the facilities had established standards for the duration and frequency of sub-threshold SpO2 levels. Assessment of pulmonary hypertension associated with BPD before and after discharge.
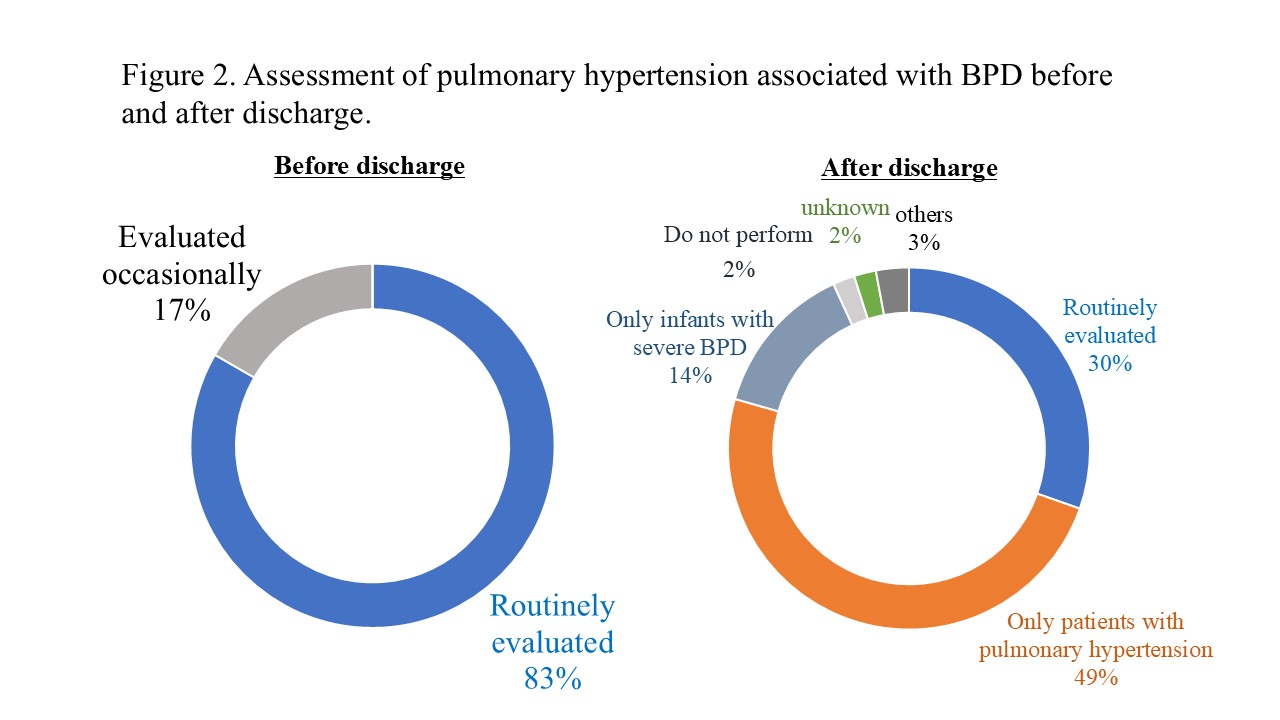 Pulmonary hypertension (PH) assessment was routinely performed in 83% of the facilities. However, only 30% of the facilities consistently conducted PH assessments after discharge.
Pulmonary hypertension (PH) assessment was routinely performed in 83% of the facilities. However, only 30% of the facilities consistently conducted PH assessments after discharge.The SpO2 threshold for discontinuing HOT and the criteria for the duration and frequency of values above that threshold.
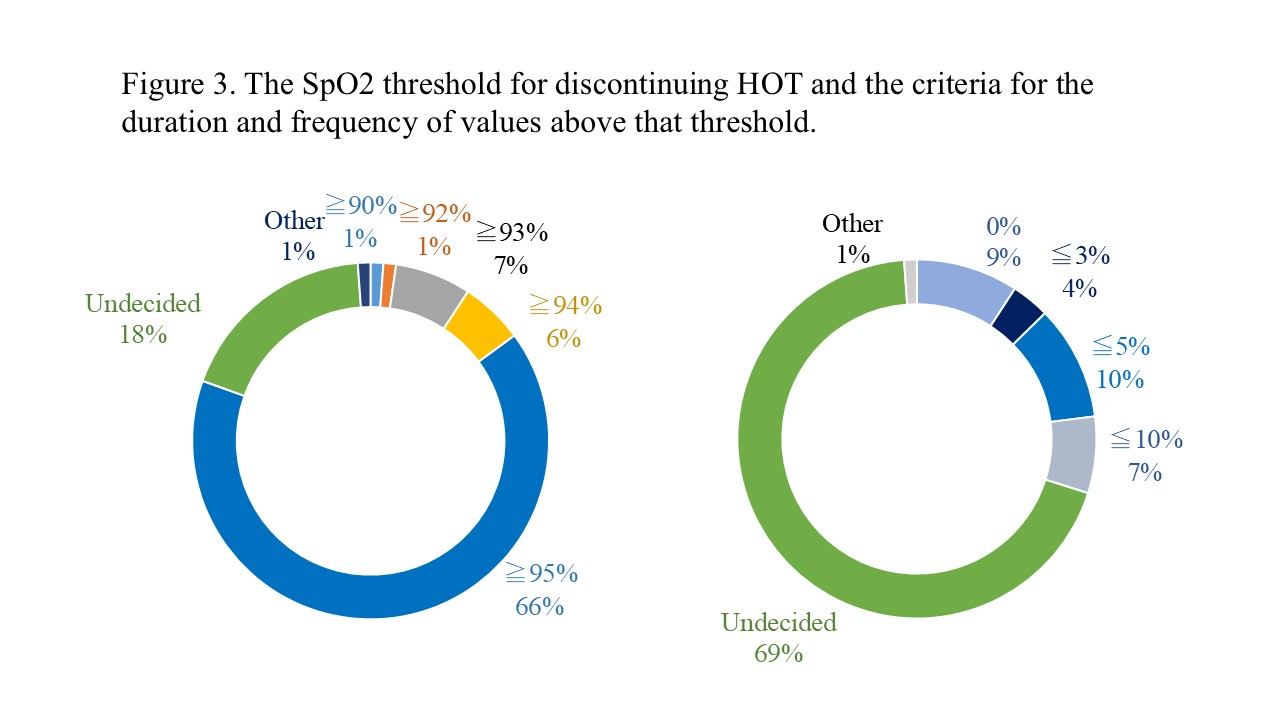 Of the facilities, 66% used a SpO2 threshold of ≥95% for discontinuation, but 69% lacked criteria for the duration and frequency of values below this threshold.
Of the facilities, 66% used a SpO2 threshold of ≥95% for discontinuation, but 69% lacked criteria for the duration and frequency of values below this threshold. 
