Neonatal Neurology 1
Session: Neonatal Neurology 1
331 - Temporal Analysis of Neonatal SpO2 Patterns Using AI Reveals Early Predictive Signatures of Severe IVH
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 331.6644
Zachary A. Vesoulis, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Rakesh Rao, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Callie Marshall, Washington University - - St. Louis, MO, St. Louis, MO, United States; Gillian C. Pet, Washington University in St. Louis School of Medicine, St. Louis, MO, United States
Zachary A. Vesoulis, MD MSCI (he/him/his)
Assistant Professor
Washington University School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Severe intraventricular hemorrhage (IVH) remains a devastating complication in preterm infants, often leading to lifelong neurological impairments. While current predictive tools have limitations, we investigated whether patterns within continuous oxygen saturation (SpO2) data could reveal early signatures of severe IVH risk.
Objective: To develop a deep learning AI model capable of analyzing continuous SpO2 signatures to discriminate preterm infants with severe IVH.
Design/Methods: We used continuous SpO2 measurements from sequential preterm infants (born Jan 2023-Sept 2024) with SpO2 captured during their first week and prospectively archived into a database (T3, Etiometry, Boston MA). Infants with IVH at birth or missing physiologic data were excluded. Our AI algorithm integrates temporal pattern recognition through Long Short-Term Memory (LSTM) neural networks and gestational age to predict severe IVH risk. The model processes SpO2 data in 5-minute segments, enabling real-time risk assessment. To enhance clinical interpretability, Gradient-weighted Class Activation Mapping (GradCAM) identified example temporal patterns driving model predictions.
Results: The study included 123 preterm infants (mean gestational age 26.0±2.1 weeks; 13 with grade 3-4 IVH). Infants who developed severe IVH demonstrated distinctive SpO2 characteristics: lower mean SpO2 (91.3% vs 93.4%, p< 0.05), higher coefficient of variation (6.49 vs 5.64%), and notably more time below critical SpO2 thresholds—below 90% (29.0% vs 19.2%, p=0.01), 85% (10.8% vs 7.0%, p=0.01), and 80% (4.9% vs 3.3%, p< 0.01).
Our model achieved an area under the receiver operating characteristic curve (AUC) of 0.855 for predicting severe IVH. Analysis revealed three key insights:
1) SpO2 patterns at various gestational age differed, with IVH cases showing consistently lower SpO2 values than those without IVH (Fig 1).
2) GradCAM analysis identified two distinct high-risk SpO2 signatures: prolonged, severe desaturations (>4 min) and periods of minimal variability in infants with severe IVH (Fig 2).
3) Model prediction confidence increased markedly by 76 hours of life, suggesting a critical intervention window and consistent with the known timing of IVH (Fig 3).
Conclusion(s): This novel application of deep learning to continuous SpO2 monitoring provides a promising approach for early identification of preterm infants at high risk for severe IVH. The model's real-time processing and interpretable results enhance its clinical potential. Future studies will focus on expanding the dataset, prospective validation, and investigating distinctions between IVH grades.
Figure 1
 In the top panel the mean SpO2 over the first 7 days is shown clustered by gestational age and outcome (no severe IVH= purple, severe IVH= gold). Despite common SpO2 alarm thresholds across the cohort (90-95%) infants at lower gestational ages achieve lower SpO2. In the bottom panel, the distribution of SpO2 values is clearly shifted lower for infants with severe IVH (gold).
In the top panel the mean SpO2 over the first 7 days is shown clustered by gestational age and outcome (no severe IVH= purple, severe IVH= gold). Despite common SpO2 alarm thresholds across the cohort (90-95%) infants at lower gestational ages achieve lower SpO2. In the bottom panel, the distribution of SpO2 values is clearly shifted lower for infants with severe IVH (gold).Figure 2
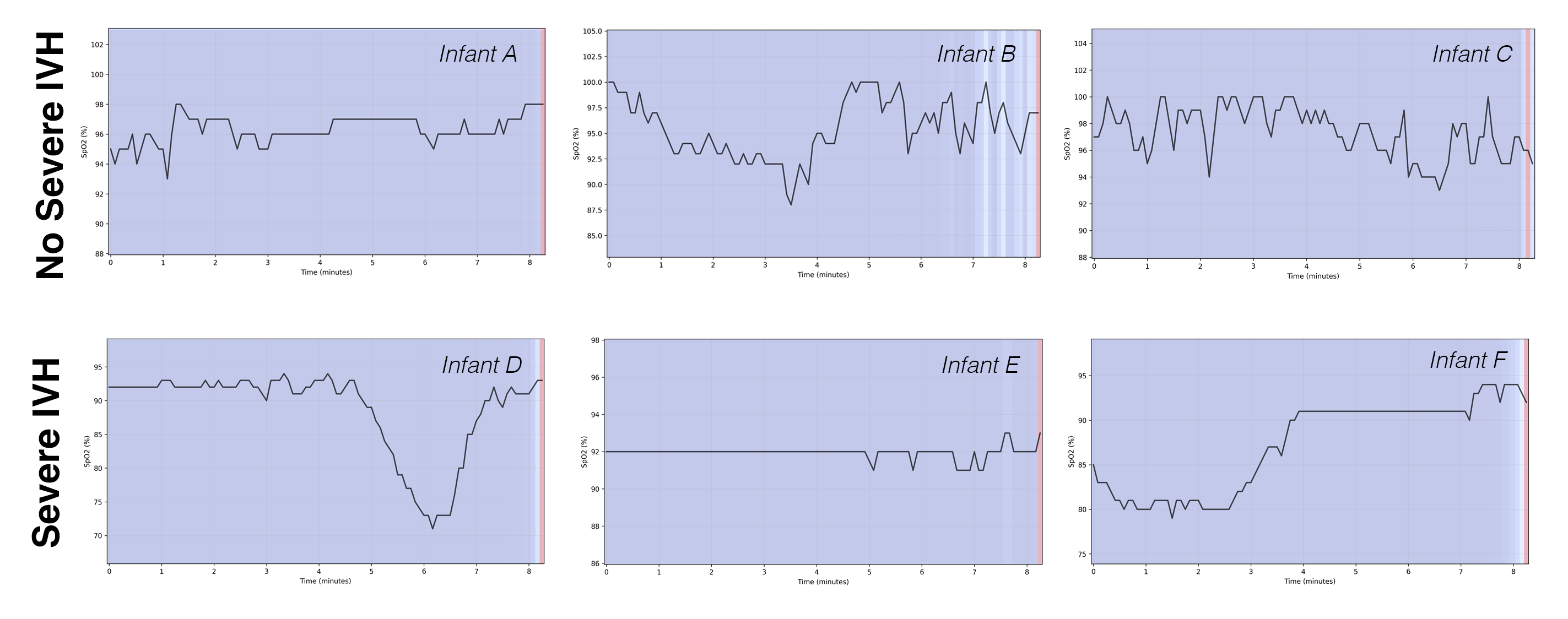 Examples of temporal patterns identified through GradCAM as predictive of severe IVH or no severe IVH outcomes. Infants A-C are noted to have saturations above 90% with consistent variability across the window. In contrast, the severe IVH infants have prolonged deep desaturations (D and F) and extremely poor SpO2 variability (E and F).
Examples of temporal patterns identified through GradCAM as predictive of severe IVH or no severe IVH outcomes. Infants A-C are noted to have saturations above 90% with consistent variability across the window. In contrast, the severe IVH infants have prolonged deep desaturations (D and F) and extremely poor SpO2 variability (E and F).Figure 3
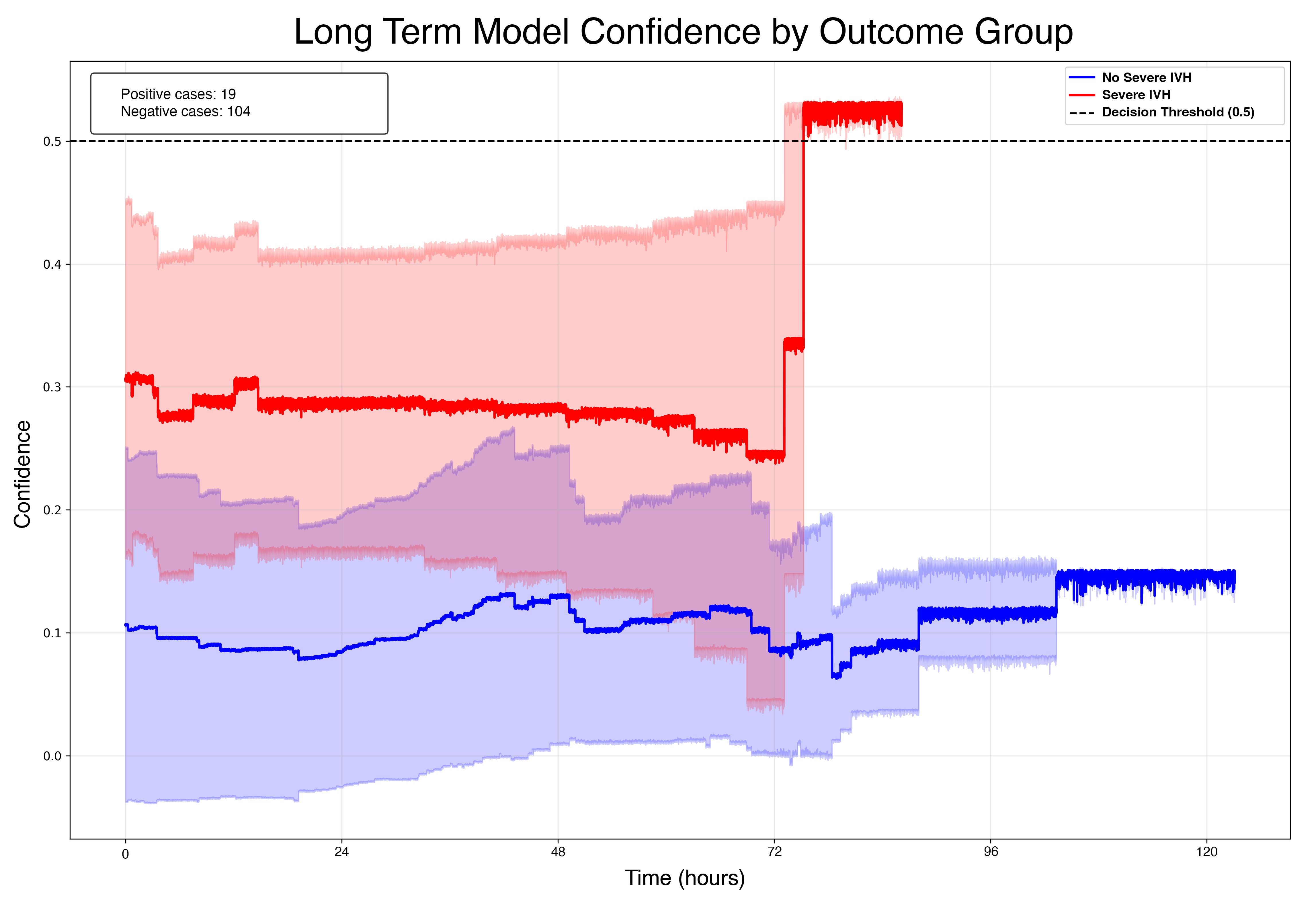 Group average confidence in outcome prediction over time. Note that the model identifies a higher risk for severe IVH immediately and reaches a confidence above threshold at approximately 76 hours (red). The model settles on a no severe IVH prediction somewhat later, on day 4 (blue). 95% confidence intervals are shown in light red and blue shading.
Group average confidence in outcome prediction over time. Note that the model identifies a higher risk for severe IVH immediately and reaches a confidence above threshold at approximately 76 hours (red). The model settles on a no severe IVH prediction somewhat later, on day 4 (blue). 95% confidence intervals are shown in light red and blue shading.
