Emergency Medicine 5
Session: Emergency Medicine 5
269 - Recognition of Significant Physical Exam findings by Pre-Hospital Providers among Children with Respiratory Distress
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 269.6123
Vincent Patrick Uy, Weill Cornell Medicine, New York, NY, United States; Eve W. Smith, Weill Cornell Medicine, New York, NY, United States; Sophie Bronstein, Weill Cornell Medicine, New York, NY, United States; Munira S. Ahmed, NYP/Weill Cornell, new york, NY, United States; Brady Rippon, Weill Cornell Medicine, Jackson Heights, NY, United States; Deborah A. Levine, Weill Cornell Medical College - New York, NY, Port Washington, NY, United States

Vincent Patrick Uy, MD (he/him/his)
Assistant Professor
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Respiratory distress is one of the most common reasons for pre-hospital providers (Emergency Medical Services or EMS) contact with pediatric patients. There is limited data regarding how well pre-hospital providers recognize significant signs of respiratory distress. Under-recognition of respiratory distress may lead to delays in treatment and higher morbidity/mortality.
Objective: To determine the agreement between the respiratory examination performed by EMS providers and that of the pediatric emergency medicine providers in children with acute respiratory distress.
Design/Methods: We performed a retrospective review of a cohort of patients aged 0-18 years of age with acute respiratory diagnosis transported by EMS to one of two pediatric EDs affiliated with an urban quaternary academic medical center from October 1, 2020 to October 31, 2023. We excluded patients who received pre-hospital treatment. A manual review of ambulance call reports and electronic medical records by three independent reviewers extracted documentation of respiratory findings such as respiratory rate, wheezing, stridor, and accessory muscle use. A modified clinical respiratory score was calculated based on the Pediatric Respiratory Score (PRS). Categorical variables were compared with McNemar’s chi-squared test with continuity correction and continuous variables by paired t-test.
Results: We reviewed 637 charts, and 234 visits met inclusion. The mean age of patients in years is 5.5 years old (Table 1). Among these visits, 28% were seen for croup, 26% were seen for anaphylaxis and 16% were seen for an asthma exacerbation. The mean transport time from origin to ED arrival was 34 minutes. Median respiratory scores were noted to be higher by PEM providers (1.36 vs 2.78). There is a significant discordance between findings of wheezing and stridor documented by EMS and PEM providers with increased recognition of wheezing and stridor by PEM physicians, in both younger and older children. (Table 2).
Conclusion(s): We found disagreement between documentation of physical signs of respiratory distress by EMS when compared to those from initial physician ED examination. Under recognition of common respiratory signs can be addressed with educational initiatives and simulation training for EMS providers.
Table 1
.png) Table 1: Demographic Information
Table 1: Demographic InformationTable 2
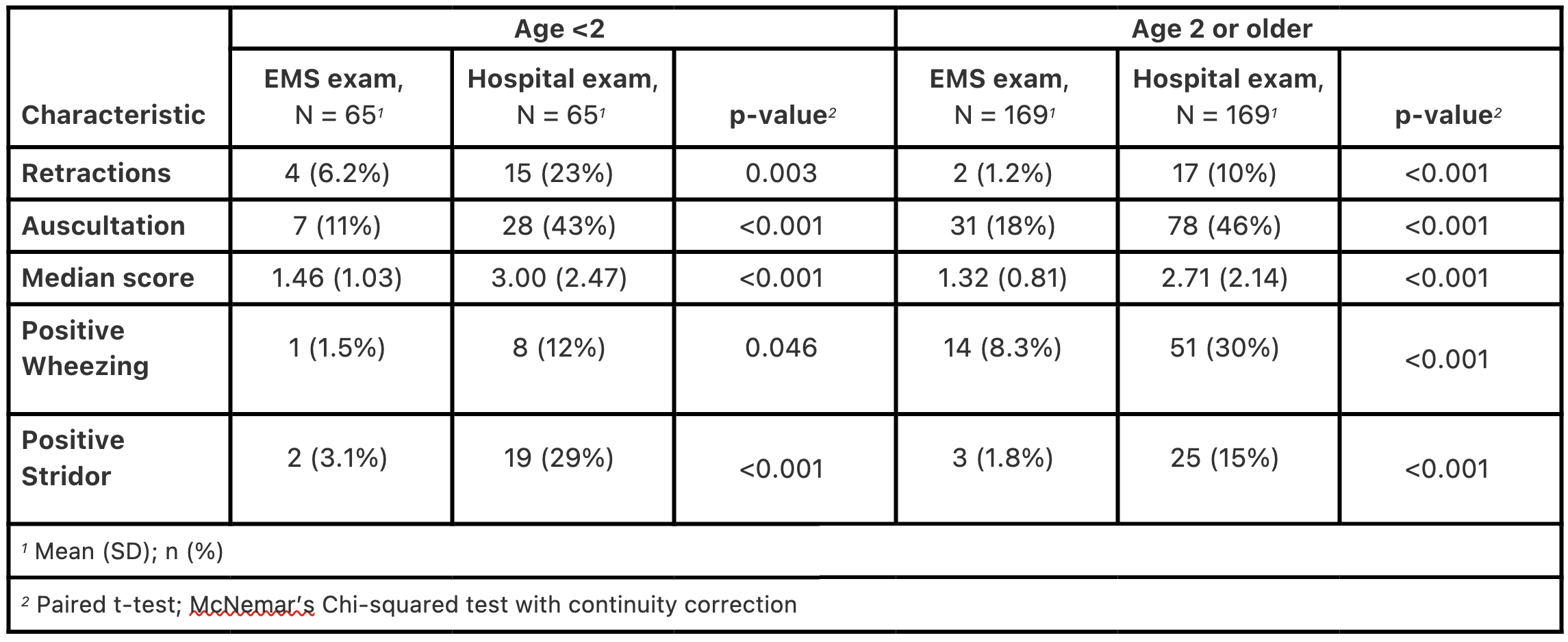 Table 2: Cross-sectional results
Table 2: Cross-sectional results Table 1
.png) Table 1: Demographic Information
Table 1: Demographic InformationTable 2
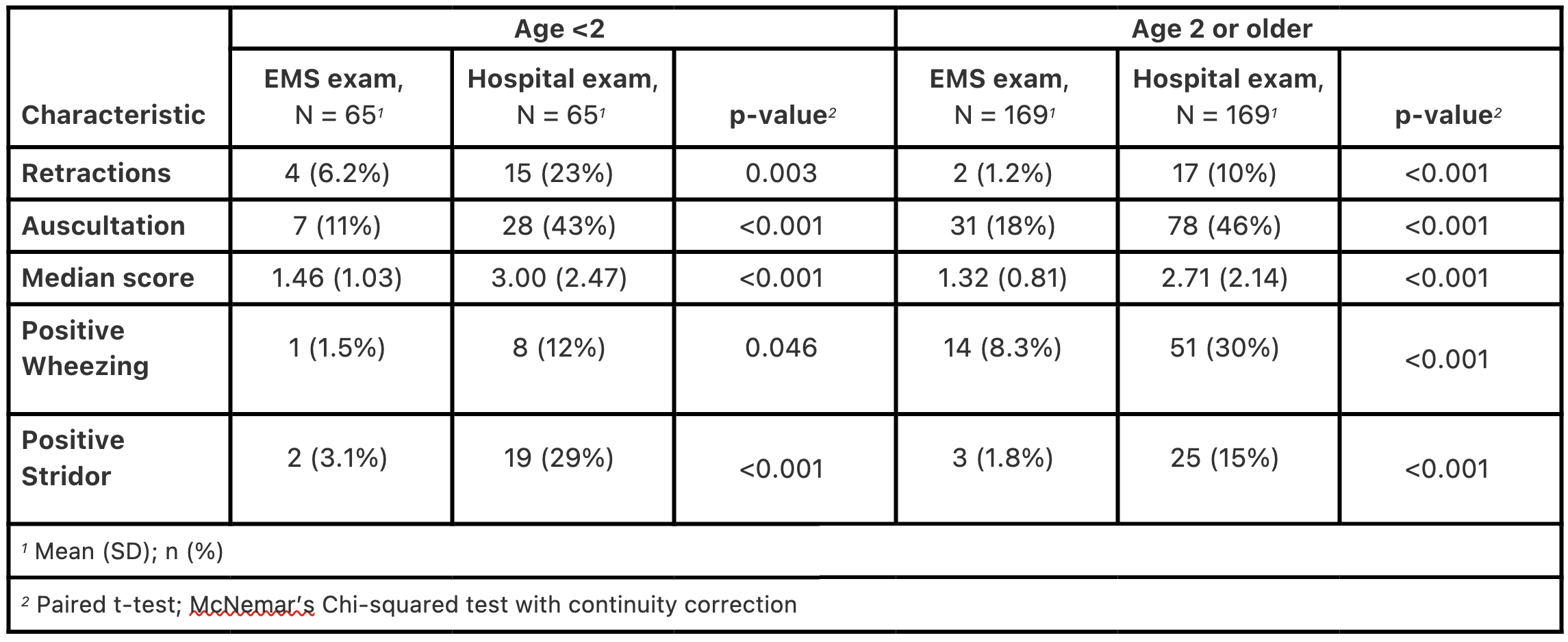 Table 2: Cross-sectional results
Table 2: Cross-sectional results 
