Mental Health 1
Session: Mental Health 1
761 - Overcoming Challenges to Implementing an Intervention for Parents of Suicidal Youth Delivered in Primary Care by a Community Health Worker
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 761.5943
Sarah Polk, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Grecia Vargas Meléndez, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Kaimy Torres-Hernandez, The Johns Hopkins Bloomberg School of Public Health, Waldorf, MD, United States; Bev Rosario-Williams, Beverlin Rosario-Williams, Washington DC 20037, US, DC, United States; Rheanna Platt, Johns Hopkins University School of Medicine, Baltmore, MD, United States; Emily Haroz, Johns Hopkins Center for Indigenous Health, Baltimore, MD, United States; Kiara Alvarez, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- SP
Sarah Polk, MD, ScM, MHS (she/her/hers)
Associate Professor of Pediatrics
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Pediatric primary care is an important venue in which to identify and mitigate suicide risk. Suicide is the third leading cause of death among 15 to 24-year-olds and the second leading cause of death among 10 to 14-year-olds.
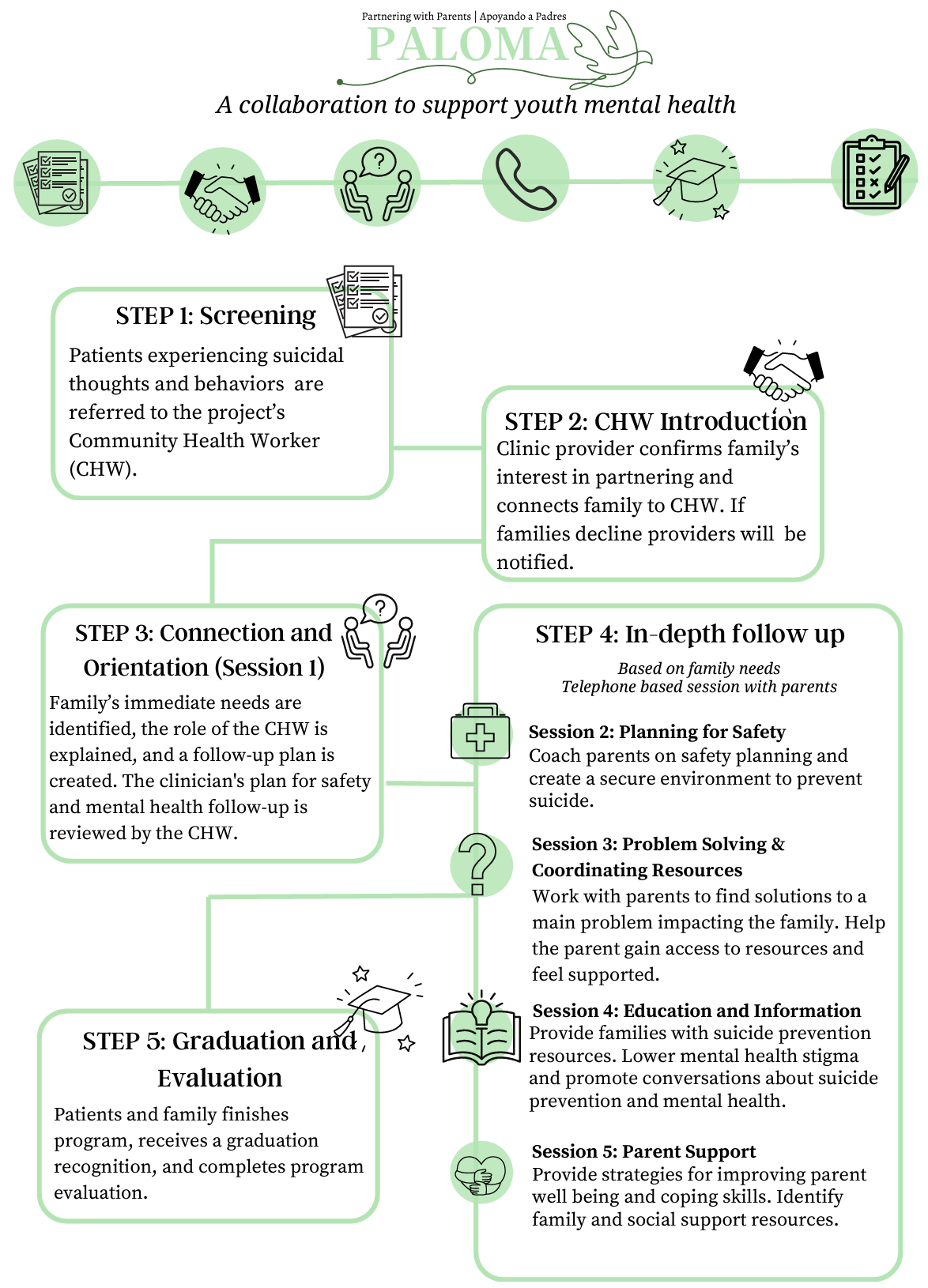
Paloma (Partnering with Parents of Adolescent Latinos on Mental Health Assistance) is an intervention for parents of youth experiencing suicidal ideation and behavior (SIB) referred by their pediatrician. The intervention consists of 5 phone calls delivered by a community health worker (CHW). It complements usual pediatric care by bolstering parental self-efficacy to engage in behaviors that promote safety, improve parent-child communication and increase parent understanding of suicide risk and prevention.
Objective: To discuss implementation barriers to the integration of a CHW-delivered support for parents of youth with SIB into pediatric primary care
Design/Methods: To discuss implementation barriers to the integration of a CHW-delivered support for parents of youth with SIB into pediatric primary care
Results: Challenges arose during screening and referral at the practice- and provider-level. Regarding screening, screeners were inconsistently handed out, practices only screened for mental health at well visits and no practice specifically screened for SIB. Regarding referral, providers had difficulty remembering the program given the relative infrequency of SIB and there was a general misperception that only youth with are at risk of suicide. Providers expressed difficulty referring eligible parents to the program when a patient had requested confidence regarding mental health problems.
Solutions to screening and referral challenges have included frequent brief updates and pearls during routine provider meetings. Efforts have been made to simplify the referral process by providing templated messages providers can send via the EMR. A library of screeners (GAD-7, PHQ-A and ASQ (Ask Suicide Questions)) have been placed in provider workplaces to serve as reminders and new mental health resources to assist providers in supporting families.
Conclusion(s): Primary care providers are increasingly responsible for managing mental health problems at the intersection of increased mental health need and insufficient specialty care resources. While the Paloma intervention was gratefully received by participating practices, we have had to overcome implementation barriers. Our lessons learned may be useful to practices taking a systematic approach to suicide risk screening and brief intervention.
Paloma intervention for Spanish-speaking parents of youth with suicidal ideation and behavior: referral process
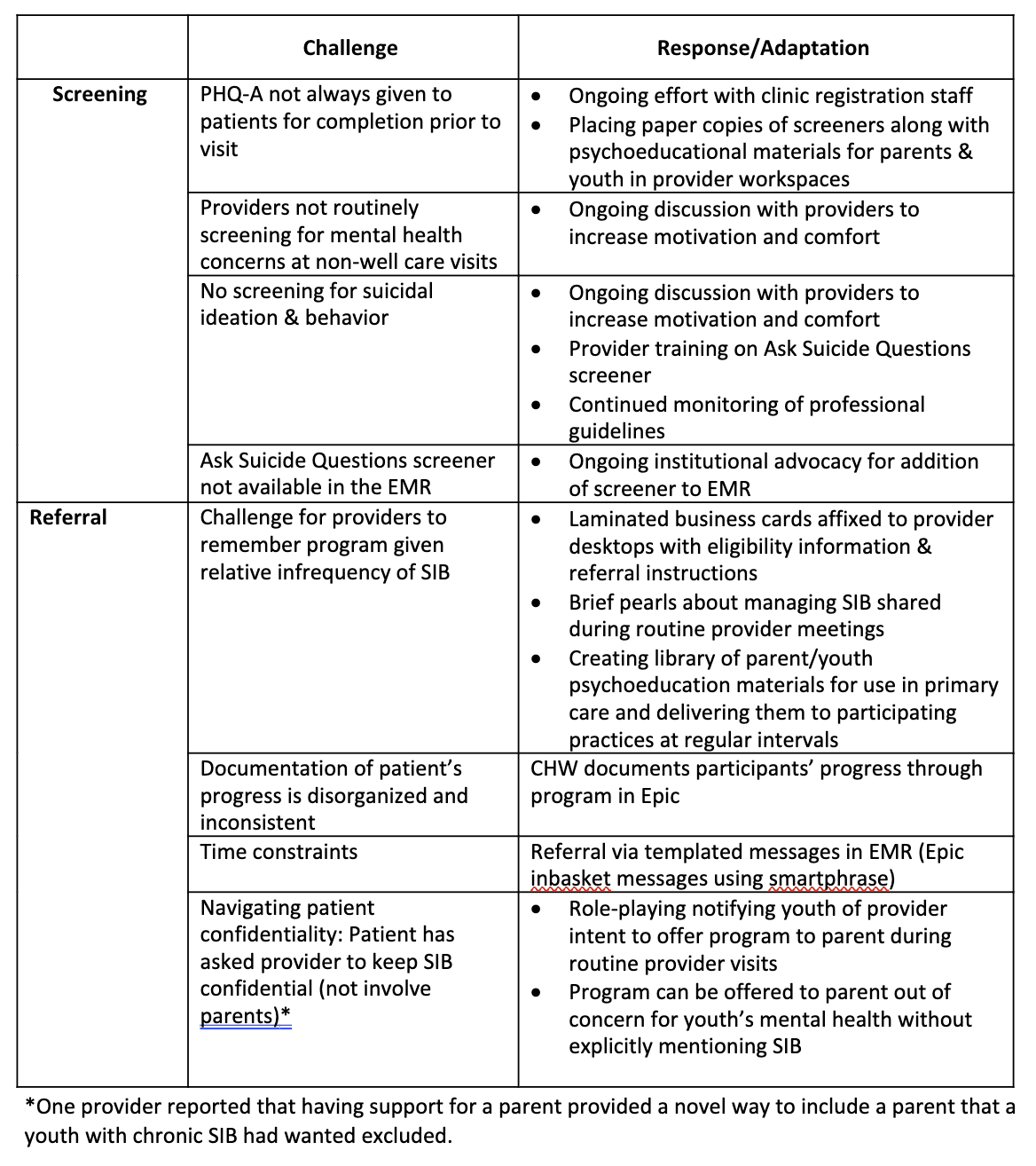
Implementation barriers to Paloma program and responses to barriers