Emergency Medicine 5
Session: Emergency Medicine 5
264 - Improving Emergency Room Post-intubation Sedation in Pediatric Patients: A Quality Improvement Initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 264.5496
Emily Wynia, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Emra Bosnjak, St. Louis Children's Hospital, St. Louis, MO, United States; Kimberly P. Mills, St., St. Louis, MO, United States; Christian M. Jackson, St. Louis Children's Hospital, St. Louis, MO, United States; Jill Whiteley, St. Louis Children's Hospital, St. Louis, MO, United States; Susan M. Wiltrakis, Washington University in St. Louis, St. Louis, MO, United States

Susan M. Wiltrakis, MD, FAAP, FACEP (she/her/hers)
Assistant Professor
Washington University in St. Louis
St. Louis, Missouri, United States
Presenting Author(s)
Background: Rapid sequence intubation (RSI) and postintubation sedation (PoISe) are essential elements in Emergency Medicine. Pediatric patients receive PoISe less frequently than adults, likely due to Pediatric Emergency Medicine (PEM) practices favoring long-acting neuromuscular blockers. Addressing this gap is vital for patient safety.
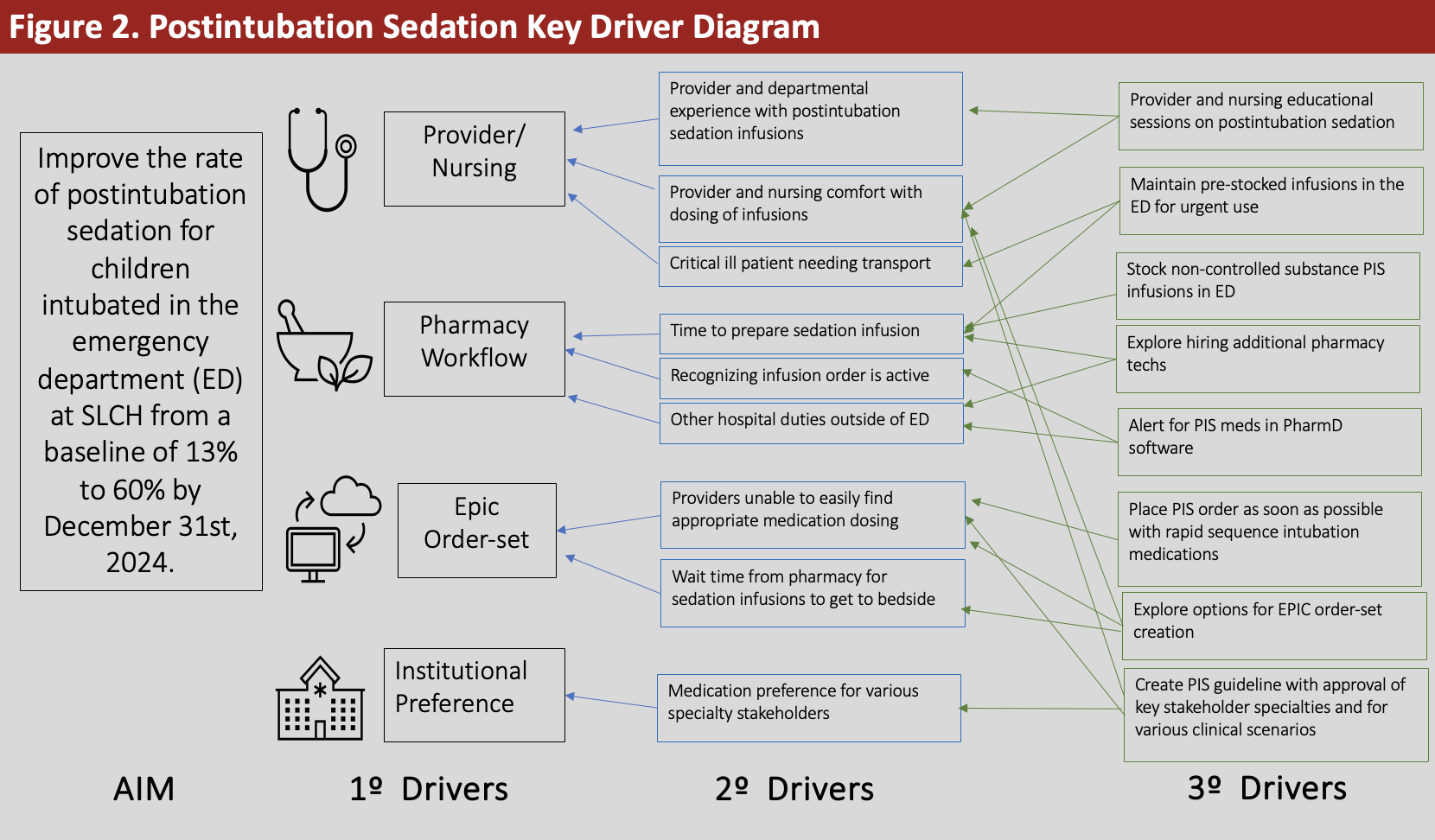
Objective: Increase continuous PoISe rates for intubated children under 18 in the SLCH pediatric ED from a median of 13% to 60% by December 1, 2024.
Design/Methods: Population includes children under the age of 18 intubated in St. Louis Children’s Hospital ED with induction paralytic, excluding pre-arrival intubations or intubations without induction paralytic. Baseline Data was collected from January 1st 2020-December 31st 2023 , calculating median number of patients receiving continuous post-intubation sedation. The Pre-Intervention Phase (June 2023-December 2023) involved creation of a process map and Key Driver Diagram, forming a PoISe QI team, and analyzing baseline data. The Intervention Phase (January 2024 – December 2024) involved interventions such as provider and nursing education (Winter 2023), PoISe guideline in February 2024, and creation and go-live of an EPIC orderset (September 2024). PDSA cycles are ongoing. Our primary measure is proportion of patients receiving continuous PoISe, and secondary measure of proporation of patient receiving PoISe within 15 minutes post-intubation. Balancing measures include ED length of stay, hemodynamic instability, and unplanned extubations.
Results: Baseline data revealed a median of 13% (15/115) of patients receiving PoISe post-intubation, with 1.7% (2/115) receiving it within 15 minutes. With QI interventions during 2023-2024, the median increased to 49% between November 2023 and October 2024. Continued data analysis is ongoing, but initial analysis does not show an increase in length of stay, instability, or unplanned extubations.
Conclusion(s): PoISe is underutilized in pediatric patients. This QI project aims to standardize PoISe practices to enhance patient safety in pediatric ED settings and initial inventions have shown improvements in utilization rates in the ED.
Figure 1: Run Chart, Post-Intubation Sedation in SLCH ED June 2023-October 2024
Figure 1- Run Chart PoISe .pdf
Key Driver Diagram: Post-Intubation Sedation