Quality Improvement/Patient Safety 6
Session: Quality Improvement/Patient Safety 6
487 - Improving Language Concordance on Discharge Instructions for Patients and Caregivers with Spanish Language Preference
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 487.5539
Morgan H. Viviano, Louisiana State University School of Medicine in New Orleans, New Orleans, LA, United States; Hope Retif, Louisiana State University School of Medicine in New Orleans, New Orleans, LA, United States; Caroline Lawless, LSUHSC New Orleans, New Orleans, LA, United States; Riley Jay, Tulane University School of Medicine, New Orleans, LA, United States; Caroline Roth, Louisiana State University Health Sciences Center, New Orleans, LA, United States

Morgan H. Viviano, MD (she/her/hers)
Resident
Louisiana State University School of Medicine in New Orleans
New Orleans, Louisiana, United States
Presenting Author(s)
Background: Pediatric patients and caregivers with non-English language preferences face several barriers to receiving equitable health care. Discharge instructions have been identified as a target to reduce these disparities. At our institution, the After Visit Summaries (AVS), which include essential return precautions and discharge instructions, are not automatically translated into patients’ preferred languages. A chart review conducted across pediatric hospital medicine and sub-speciality services over 15 months revealed that only 10% of return precautions for patients with Spanish language preference (SLP) were provided in Spanish.
Objective: To increase the percentage of language concordant return precautions for patients with SLP from 10% to 50% in 6 months.
Design/Methods: The primary outcome measure was percentage of patients with SLP who received language-concordant return precautions. Process measures included use of a language-concordant smart phrase or checkbox for return precautions and resident awareness of these tools. The balancing measure assessed resident perception of the effort required to provide language-concordant information to patients with SLP. Data for measures were collected via review of 10 charts of patients with SLP per month and via a survey of senior residents.
For PDSA cycle 1, a Smart Phrase within our electronic medical record was created listing standard return precautions in Spanish and English with the aid of our institution’s translation services provider. This smart phrase was distributed to residents in multiple forms. For PDSA cycle 2, the smart phrase was incorporated into an automatically displayed check-box option within the discharge order set in order to facilitate use.
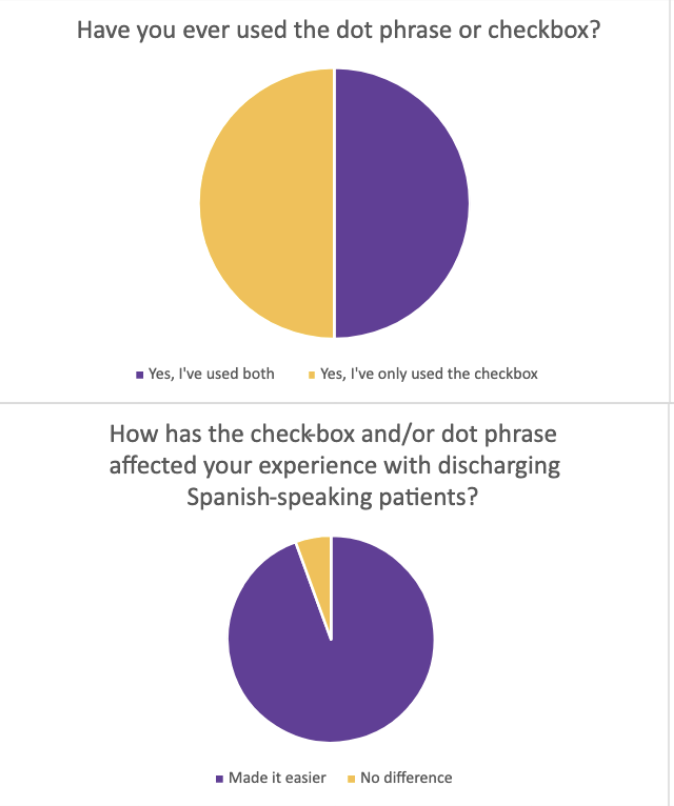
Results: We surpassed our primary aim by increasing language-concordant Spanish return precautions from 10% to 90% within 6 months. The project has maintained success over 15 months post-intervention, with an average usage rate of 65%. Additionally, a survey of 18 pediatric residents showed 100% awareness and utilization of the resource; 94% indicated that the checkbox facilitated the discharge process, and 100% believed the intervention added value to the return precautions provided to patients.
Conclusion(s): Employing a simple change to our discharge order set, we have been able to maintain our goal of providing more equitable return precautions to our patients. Moving forward, we aim to sustain and improve the percentage of language concordant return instructions and to pursue expansion of its use to other departments including Internal Medicine and Pediatric General Surgery.
Chart 1: Run Chart of Percent Language-Concordant Return Precautions Provided During Study Period
.png) Chart includes monthly data collection with 15 points pre-intervention and 15 post-intervention. Initiation of PDSA cycles 1 and 2 are indicated on the chart, and a running average following intervention is outlined in orange.
Chart includes monthly data collection with 15 points pre-intervention and 15 post-intervention. Initiation of PDSA cycles 1 and 2 are indicated on the chart, and a running average following intervention is outlined in orange. Chart 2: Pie Charts Depicting Resident's Responses to Post-Intervention Survey