Medical Education 5: Procedures and Simulation
Session: Medical Education 5: Procedures and Simulation
228 - Defining Competency in Airway Management in Pediatric Subspecialty Trainees
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 228.4275
Rebecca J. Martin, Arkansas Children's Hospital, Little Rock, AR, United States; Chinyere Egbuta, Harvard Medical School, Boston, MA, United States; Ron Sanders, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Michael Anders, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Martha Rojo, University of Arkansas for Medical Sciences College of Nursing, Little Rock, AR, United States; Akira Nishisaki, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Rebecca J. Martin, MD, MHPTT
Fellow
Arkansas Children's Hospital
Little Rock, Arkansas, United States
Presenting Author(s)
Background: Airway management is a core skill for pediatric critical care medicine (PCCM), pediatric emergency medicine (PEM) physicians and neonatologists. Intubation in critically ill children is a high-risk procedure. Adverse events occur more often when airway management is performed by those with less experience. The American Board of Pediatrics and Accreditation Council for Graduate Medical Education established standards for pediatric subspecialty fellows using entrustable professional activities, competencies, milestones. However, these standards are not specific to airway management.
Objective: We aimed to define competency measures in airway management for pediatric subspecialty trainees.
Design/Methods: Modified Delphi methodology was used to survey 20 physician educators identified through the National Emergency Airway Registry for Children (NEAR4KIDS) with expertise in PCCM, PEM, or neonatology. Consensus was defined as 80% or more of respondents in agreement. Descriptive statistics were used to analyze quantitative Delphi questionnaire responses. Narrative responses were reviewed using inductive and deductive content analysis by 2 independent team members. Disagreements were resolved by consensus with a third team member confirming overall themes.
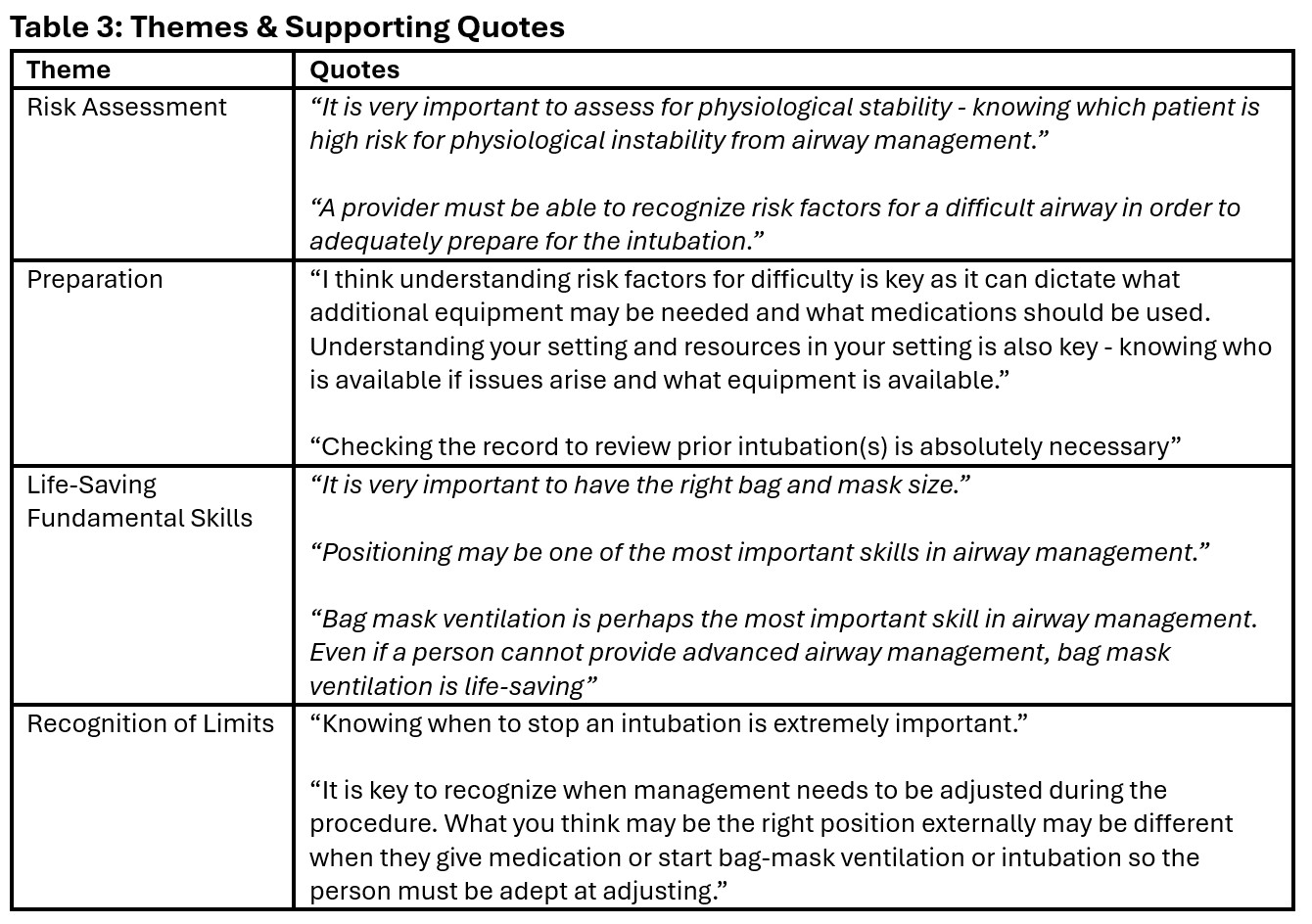
Results: Response rate was: first round 12/20 (60%) and second round 13/20 (65%). Some respondents practiced in multiple subspecialties, such as pediatric anesthesia/critical care medicine (Table 1). 32/47 (68%) achieved consensus in the first round. 5 statements were refined from comments. 7/16 (44%) statements achieved consensus in the second round, resulting in a total of 39 consensus statements (Table 2). Each category had 3-12 statements; endotracheal intubation had the largest statement count. Categories were refined based on content analysis. Competency statements that did not reach consensus included laryngoscopy methods (direct vs video), acceptable number of intubation attempts. Content analysis revealed themes of risk assessment, preparation, life-saving fundamental airway skills, and recognition of limits as vital to comprehensive, team-based care for the critically ill child (Table 3).
Conclusion(s): Experienced physicians with expertise in pediatric airway management and graduate medical education agree that airway management skills rely on fundamental exam and assessment skills, preparation, and teamwork. However, our physician-educators did not agree on the role of technology in airway management skill acquisition. This reflects the variable uptake of new technology in medical education.
Table 1: Respondents' Subspecialty Expertise
.jpg)
Table 2: Consensus Statements on Pediatric Airway Management Competency
.jpg)
Table 3: Themes & Supporting Quotes