Health Equity/Social Determinants of Health 2
Session: Health Equity/Social Determinants of Health 2
414 - Care Preferences and Support Needs for Birthing People: A Mixed-Methods Study to Inform Dyadic Perinatal Care
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 414.4285

Nicole C. Amodio, MPH (she/her/hers)
Research Assistant
Yale School of Medicine
Phoenix, Arizona, United States
Presenting Author(s)
Background: Timely, accessible prenatal and postpartum healthcare supports the health and well-being of the birthing parent-infant dyad, enabling detection and prevention of pregnancy-related complications and chronic conditions. As U.S. maternal mortality and morbidity disproportionately affects Black and Hispanic women, adopting focused, intentional dyadic care informed by community perspectives can improve healthcare access and mitigate inequities.
Objective: To understand factors influencing access to and effectiveness of perinatal health for the birthing person-infant dyad by exploring perspectives and healthcare preferences, identifying pregnancy and postpartum health knowledge, and discerning opportunities to empower birthing people to promote health advocacy.
Design/Methods: In this mixed-methods study, our interdisciplinary team administered an iteratively developed interview guide and survey with English/Spanish-preferred speakers who received care at a maternal-child mobile health van or a Postpartum Heart Health program. We purposively sampled from health centers where most patients receive Medicaid insurance. Phone interviews were recorded via HIPAA-compliant videoconference. Interviews, transcribed with automated software, were edited by research team members. A four-person coding team (two of whom speak Spanish), coded transcripts in original languages in Dedoose. Discrepancies were resolved by consensus, and the constant comparative method was applied to identify emerging themes. Descriptive statistics were applied to quantitative data.
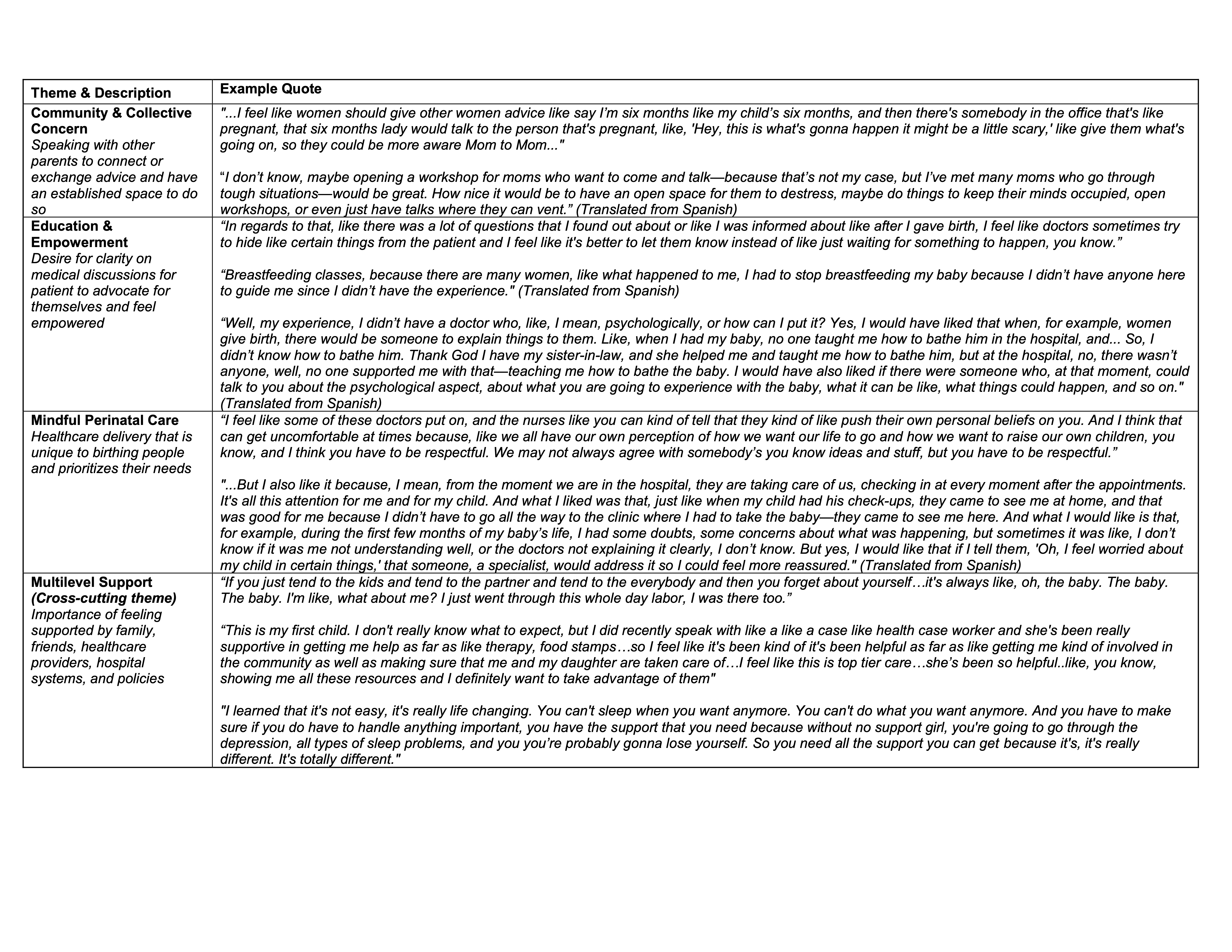
Results: Of the 22 in-depth interviews (9 Spanish,13 English) (Table 1), half chose either a home visit or a van visit as their preferred care setting, and half reported a missed clinic-based appointment due to transportation (Table 2). Key themes reflected postpartum healthcare priorities: 1) multi-level support centered around birthing person-infant dyad preference; 2) need for connection and belonging in the broader community; 3) improved provider communication and education to empower self-care and health knowledge; and 4) healthcare recognition of and response to the needs and desires of birthing persons.
Conclusion(s): Birthing people’s perspectives reflected the need for multilevel support with specific attention to community and relationship strengthening, provider engagement, and policy opportunities. To improve patient interactions with healthcare systems, future care innovations addressing disparities in perinatal health outcomes would benefit from incorporating holistic, patient-centered perspectives.
Table 1. Respondent characteristics (n = 22)
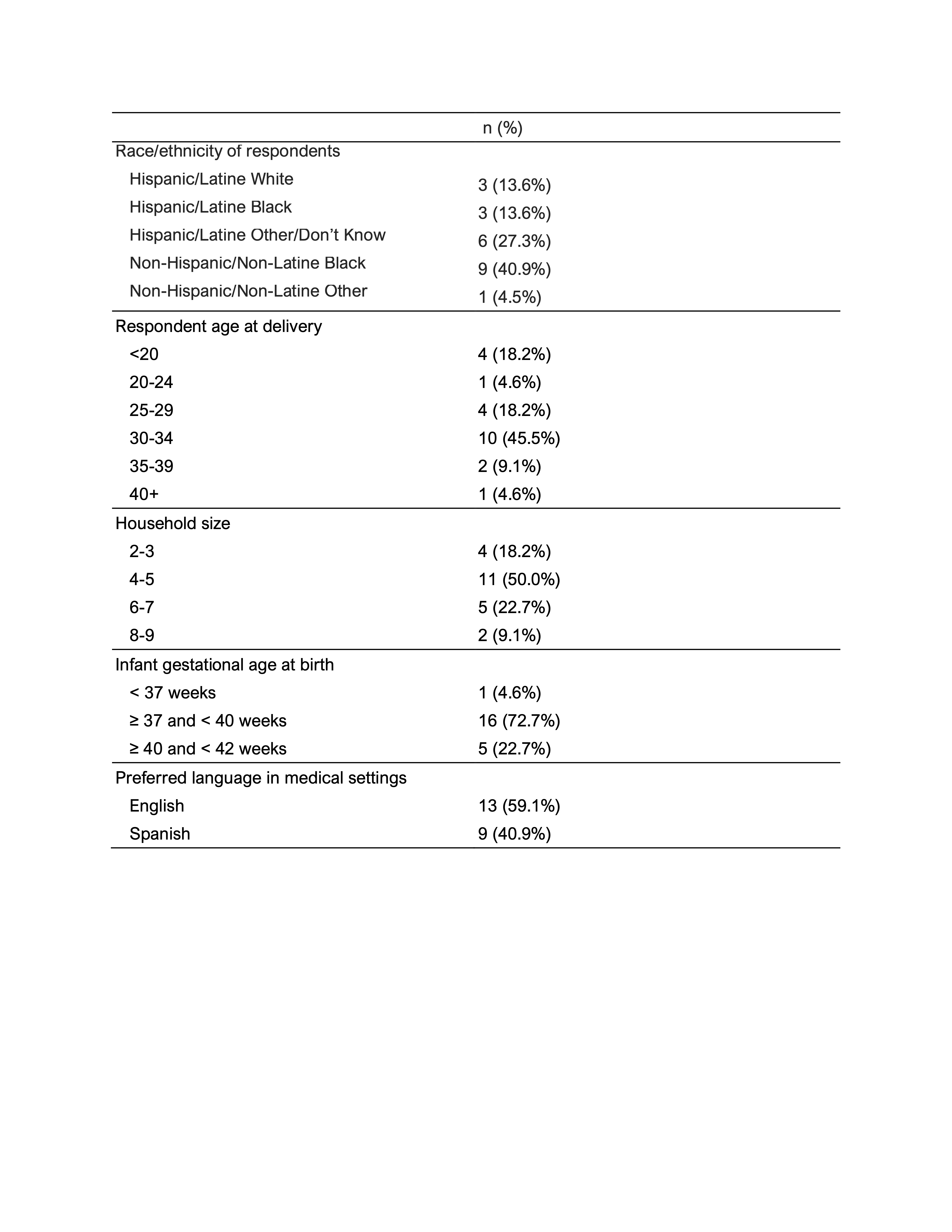
Table 2. Patterns of postpartum care receipt
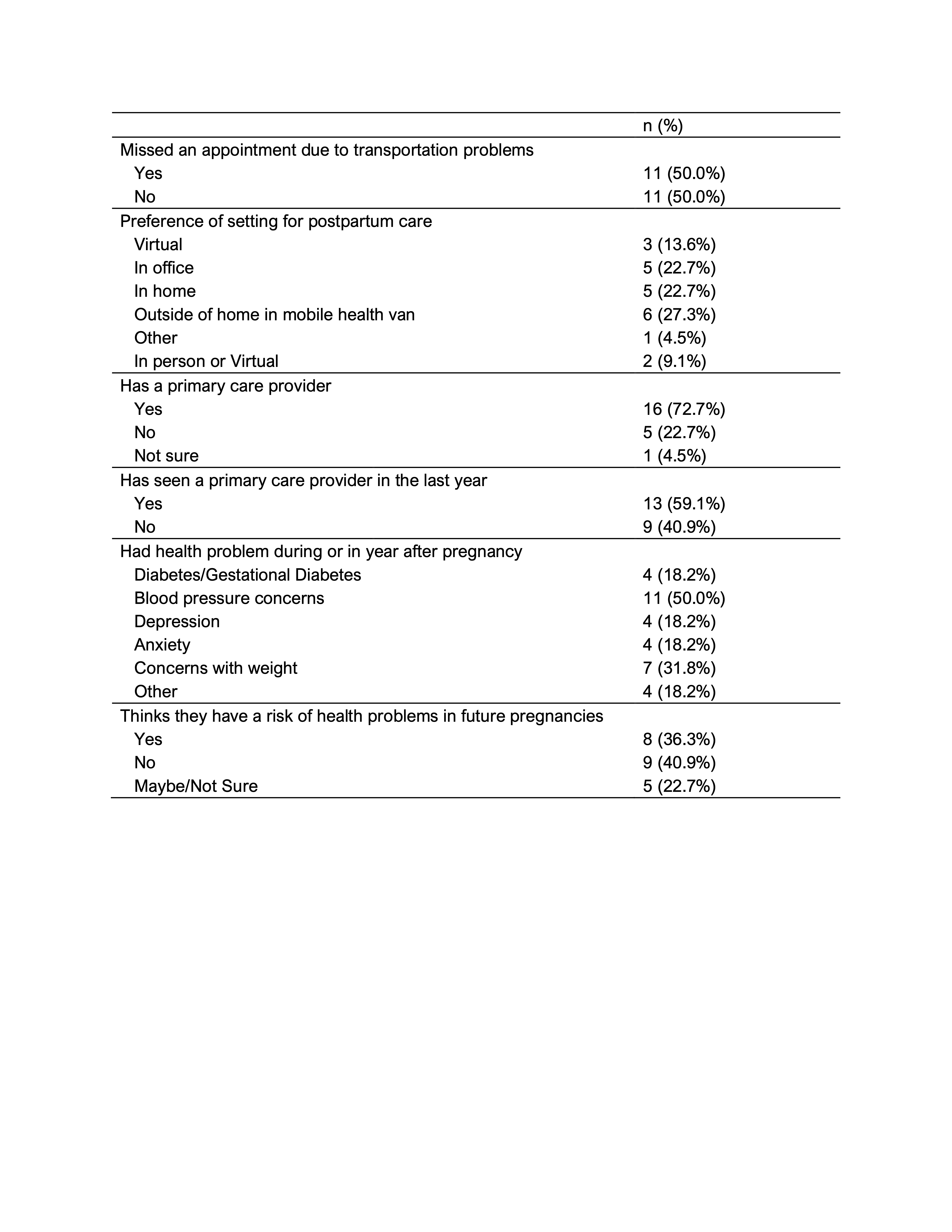
Table 3. Themes and representative quotations from qualitative discussions