Pediatric Nutrition
Session: Pediatric Nutrition
737 - Child Opportunity Index Does Not Impact the Safety and Efficacy of Home NG Tube Feeding in Premature Newborn Babies Born at a Rural Academic Medical Center
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 737.4267
Karina Lukovits, Geisel School of Medicine at Dartmouth, NORWICH, VT, United States; Kathryn Richards, Dartmouth Health Children's, Lebanon, NH, United States; William L. Daugherty-Miller, Dartmouth Hitchcock Medical Center, Keene, NH, United States; Tyler k. Hartman, Geisel School of Medicine at Dartmouth, Lebanon, NH, United States; Reto M.. Baertschiger, Children's Hospital at Dartmouth-Hitchcock, Lebanon, NH, United States

Karina Lukovits, BSc (she/her/hers)
Medical Student
Geisel School of Medicine at Dartmouth
NORWICH, Vermont, United States
Presenting Author(s)
Background: Our center’s Hope Grows at Home (HGH) Program has shown that preterm infants with nasogastric (NG) feeding tubes can be feasibly cared for at home with remote patient monitoring and telehealth support. Early discharge programs are becoming more popular, as they decrease morbidity and costs associated with hospital stays, and may reduce invasive procedures (eg. gastrostomies). However, it is unclear whether particular patient characteristics or socioeconomic factors impact the success of such programs in rural settings.
Objective: Determine whether multiple gestation status and socioeconomic status (defined by Child Opportunity Index; COI) affect home NG feed duration in a cohort of preterm infants born at a rural center.
Design/Methods: An IRB-approved retrospective chart review was performed of 100 premature infants consecutively enrolled in the HGH program from July 2020 to November 2023. The program involved remote patient monitoring and telehealth support for premature infants discharged with NG feeds. Demographics, multiple gestation status, distance to the hospital, COI based on zip code, and other clinical outcomes were recorded. Statistical analyses included Mann-Whitney U tests, one-way ANOVA, Spearman's correlation coefficients, and multiple linear regression, with significance defined at p< 0.05. Results are presented as mean (standard deviation SD).
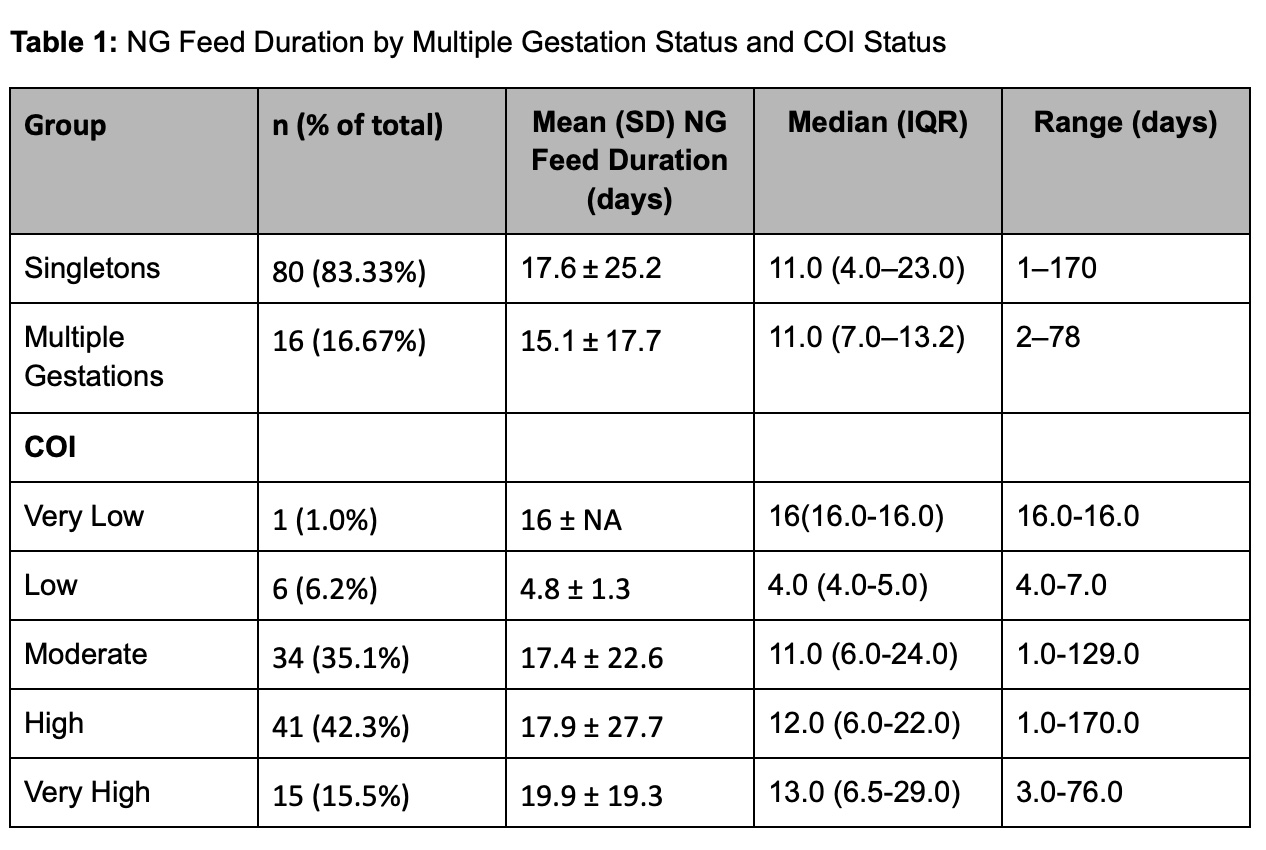
Results: Ninety-six patients (59% female) were analyzed (4 incomplete records). Mean gestational age at birth was 32.99 weeks (SD 2.99). Mean birth weight was 1.91kg (SD 0.62). Sixteen patients (16.7%) were products of multiple gestations. Mean NG duration was 17.2 days (SD 23.6). Average distance from the hospital was 49.1 miles (SD 25.3). Three patients required gastrostomies and 3 patients were readmitted for reasons unrelated to feeding.
There was no significant difference in NG duration between multiple gestation infants and singletons (mean 15.1 days vs. 17.6 days; p=0.931). Higher gestational age at birth was significantly correlated with reduced NG duration (p=0.017). COI status was not significantly correlated with NG duration (p=0.244) or readmission rates (p=0.876). Multiple regression analysis controlling for gestational age, birth weight, and distance from hospital confirmed these results.
Conclusion(s): These results suggest that home NG feeding programs can be safely implemented for preterm infants of multiple gestational status and from diverse socioeconomic neighborhoods. Thus, such programs are appropriate for families that would likely benefit the most from avoiding the financial and emotional strain of a prolonged hospital course.
Table 1: NG Feed Duration by Multiple Gestation Status and COI Status