Medical Education 7: DEI
Session: Medical Education 7: DEI
455 - Development of an Interprofessional Group-Based Mentorship Program for BIPOC Participants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 455.4339
Anisha Rimal, Hennepin County Medical Center, Minneapolis, MN, United States; Molly Rideout, The University of Vermont Children's Hospital, Burlington, VT, United States; Miller Celestin, University of Pennsylvania, School of Nursing, Center for Health Outcomes and Policy Research, Philadelphia, PA, United States; Sarah Manacek, Robert Larner, M.D., College of Medicine at the University of Vermont, Burlington, VT, United States; Anthony R. Williams, University of Vermont, Williston, VT, United States; Thomas Delaney, University of Vermont Larner College of Medicine, Montpelier, VT, United States

Anisha Rimal, MD (she/her/hers)
Assistant Professor of Pediatrics
University of Minnesota School of Medicine
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: An important strategy to address health inequities is to establish a more diverse healthcare workforce. Programs that seek to retain and support healthcare trainees and faculty from underrepresented in medicine (UIM) groups are critical. At our institution, there was no mentorship program that offered racially concordant mentorship for BIPOC (black, indigenous, person of color) medical or nursing students.
Objective: Following the development of a group-based, interprofessional mentorship program for BIPOC mentors and mentees, this study seeks to assess: 1) Changes in “sense of belonging” scores for participants, and 2) Changes in mentorship competency scores for program mentors. Data collection from a second cohort of participants is ongoing.
Design/Methods: Program participants included BIPOC medical and nursing students, nursing and physician faculty, and medical trainees. Participants were divided into “clusters” composed of faculty mentors, near-peer mentors, and student mentees. Program activities included monthly small-group meetings, quarterly social events drawing on BIPOC community-building infrastructure, and professional development opportunities for mentors. Participants completed a pre and post program validated survey that queried their sense of belonging. Mentors completed pre and post Mentorship Competency Assessments (MCAs). Average pre vs post item scores were calculated for each category for both survey types. T-tests (2 tailed) were performed to determine statistical significance of pre/post score difference.
Results: On baseline sense of belonging scores (Table 1) BIPOC students had significantly lower overall scores than non-BIPOC students (p < 0.01). For mentor sense of belonging, post-survey results showed an average increase of 0.1 compared to baseline, which was not statistically significant. MCA mean scores increased by 0.2 (non-significant) in the post-survey results, however the increase in the Assessing Understanding MCA domain (4.2 to 5.2) approached significance (table 2). Only 6 student mentees completed the post surveys, thus meaningful comparisons were not able to be performed.
Conclusion(s): A group-based, interprofessional mentorship program is an innovative model to provide support for BIPOC health professions students. For mentors in our program, both sense of belonging scores and mentorship competency scores increased following the first year of the program. Group-based mentorship models may be an effective means to better support BIPOC health professions students and faculty, with the goal of improving retention and recruitment of a diverse healthcare workforce.
Table 1
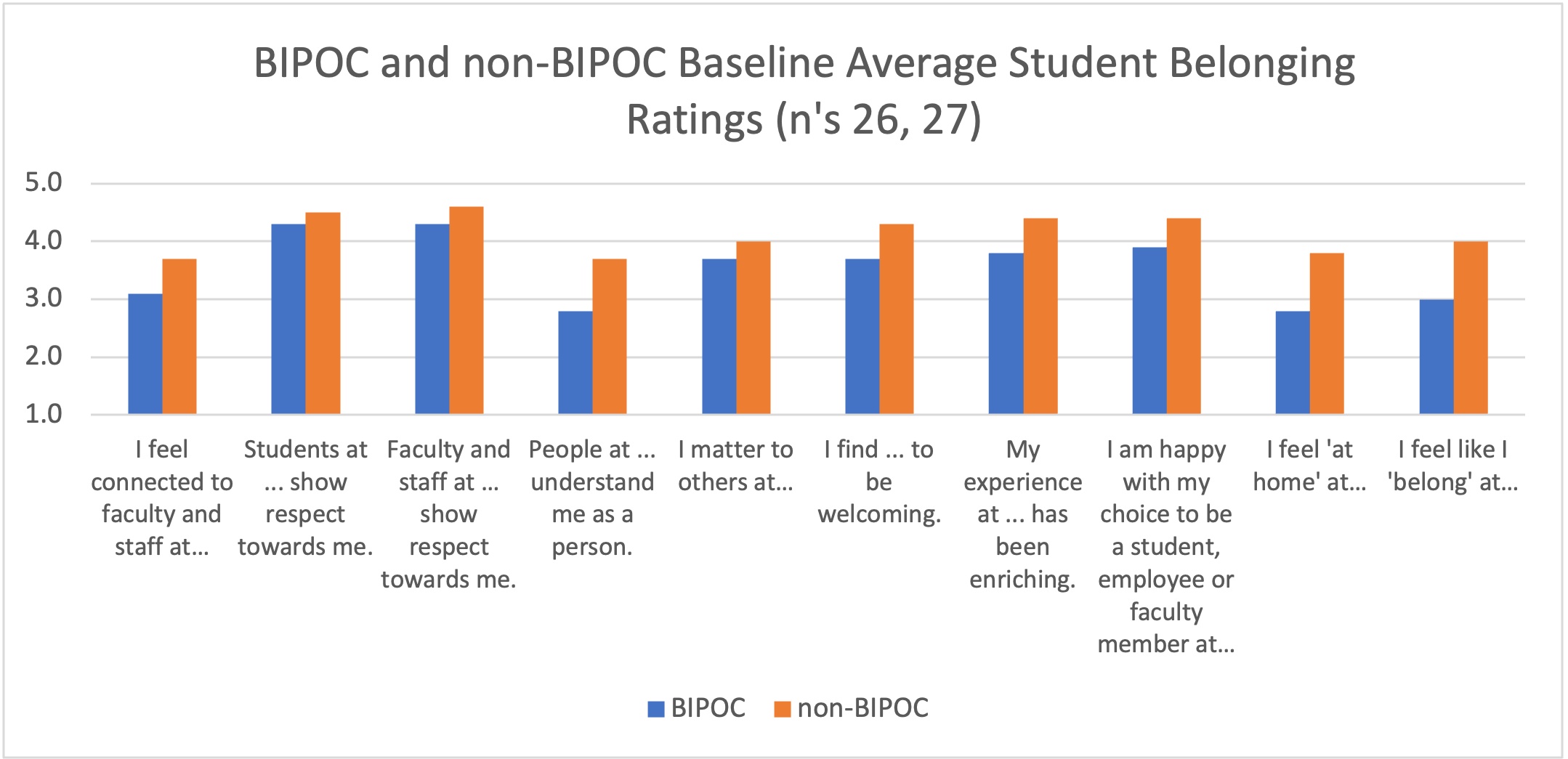 Student Sense of Belonging (Baseline)
Student Sense of Belonging (Baseline)Table 2
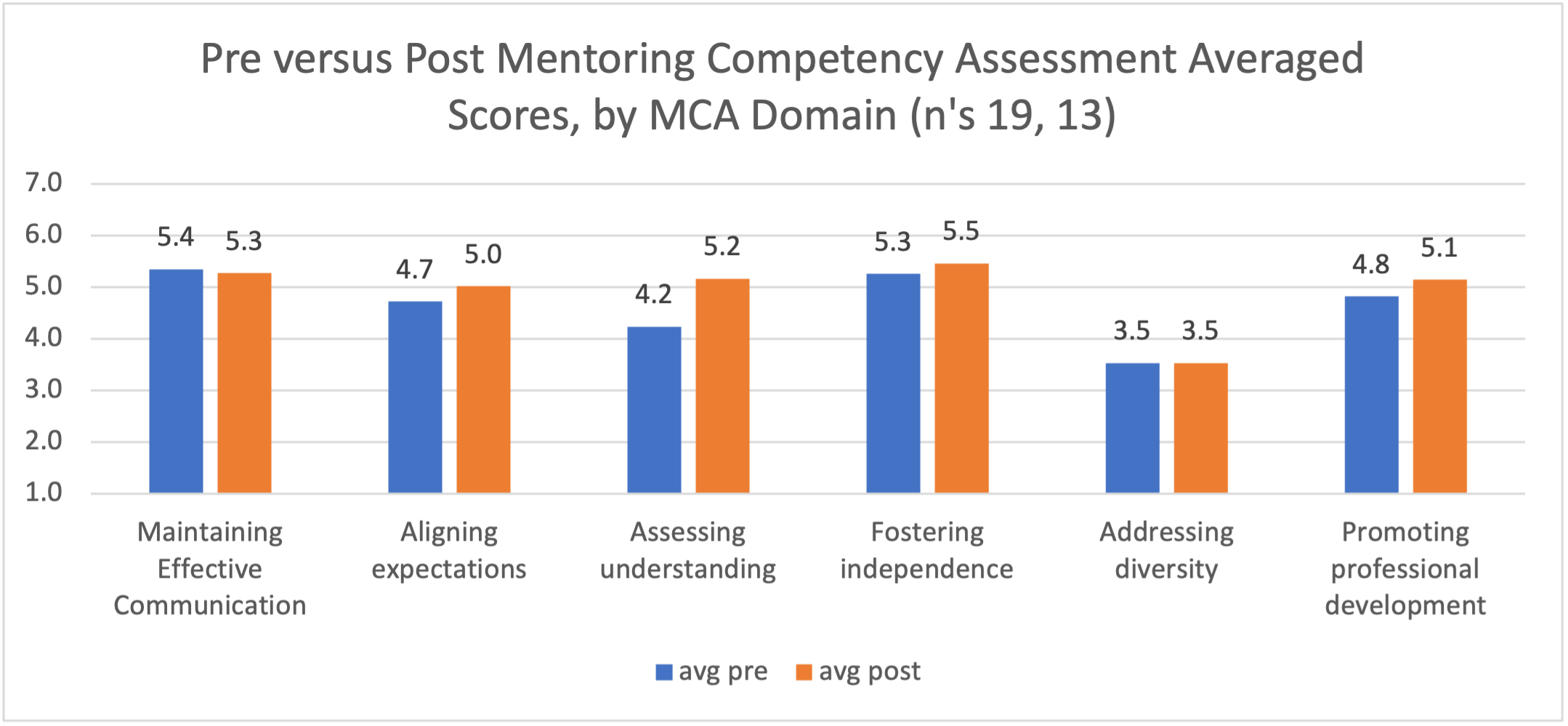 Mentorship Competency Assessment (Post)
Mentorship Competency Assessment (Post)
