Emergency Medicine 5
Session: Emergency Medicine 5
268 - Pediatric Death in the Emergency Department: Qualitative Insights from Physicians’ Experiences
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 268.5684
Ji Young Lee, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Jamie Pattee, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Christine Aspiotes, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Maren M. Lunoe, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Traci M. Kazmerski, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Noel B. Spears, UPMC CHP, Pittsburgh, PA, United States; Kathleen A.. Noorbakhsh, University of Virginia School of Medicine, Charlottesville, VA, United States
Ji Young Lee, MD (she/her/hers)
Fellow
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: The death of a child is a rare and high-stress event in the pediatric emergency department (ED). Management of pediatric death in the ED is hard to standardize as each situation presents with unique characteristics and challenges. It is essential to reflect on these experiences to enhance the process and provide support for the physicians involved in the death of a child in the ED.
Objective: We explored ED physician perspectives related to the death of a child to identify key lessons and areas for improvement.
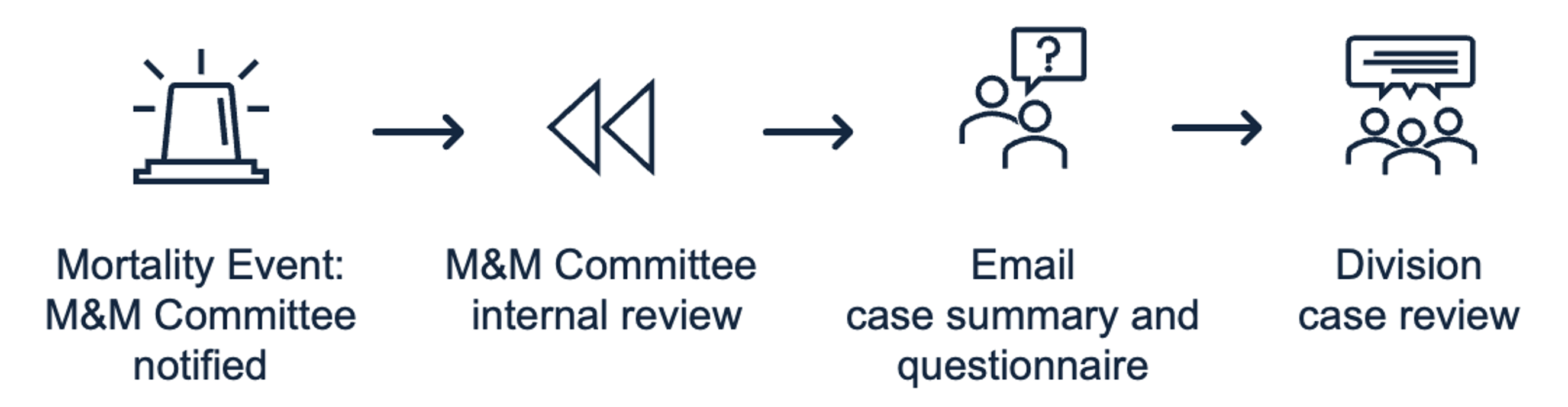
Design/Methods: We conducted a five-year retrospective review of survey responses from pediatric emergency medicine physicians after the death of a child at a single center. The division’s morbidity and mortality committee reviews every death, documents a standardized case summary, and asks the following free-text questions (Figure 1): 1) Are there any additional items you would like to discuss about the resuscitation? 2) Do you have any thoughts or comments on your team debrief? 3) Did you feel supported during and after running this resuscitation? 4) Based on this experience, is there anything that could be changed to improve the resources or information available during a resuscitation in the ED? We collected respondent demographic information, including gender and clinical experience. Using qualitative software, we analyzed free-text responses and identified key themes and representative written excerpts.
Results: During the study period, there were 80 ED deaths and 34 survey respondents (43% response rate). Among respondents, 56% (19/34) were women and 44% (15/34) had greater than five years of clinical experience (Table 1). Preliminary analysis uncovered the following key themes: 1) The majority of physicians found it helpful to have multidisciplinary providers with different expertise present during the resuscitation; 2) Family involvement was vital and impactful during and after the death of a child; 3) Continued support during and after the death of a child was crucial for returning to normal ED operations; 4) Staff debriefings occurred frequently and were greatly valued, but did have barriers to implementation.
Conclusion(s): This study provides a unique perspective on the factors that physicians consider significant in the death of a child in the ED. Results highlight the importance of providing continued support and opportunity to debrief. Future studies should seek to include insights from non-physician healthcare providers and family members, while also exploring the emotional aspects involved when a child dies.
Table 1 Characteristics of Respondents
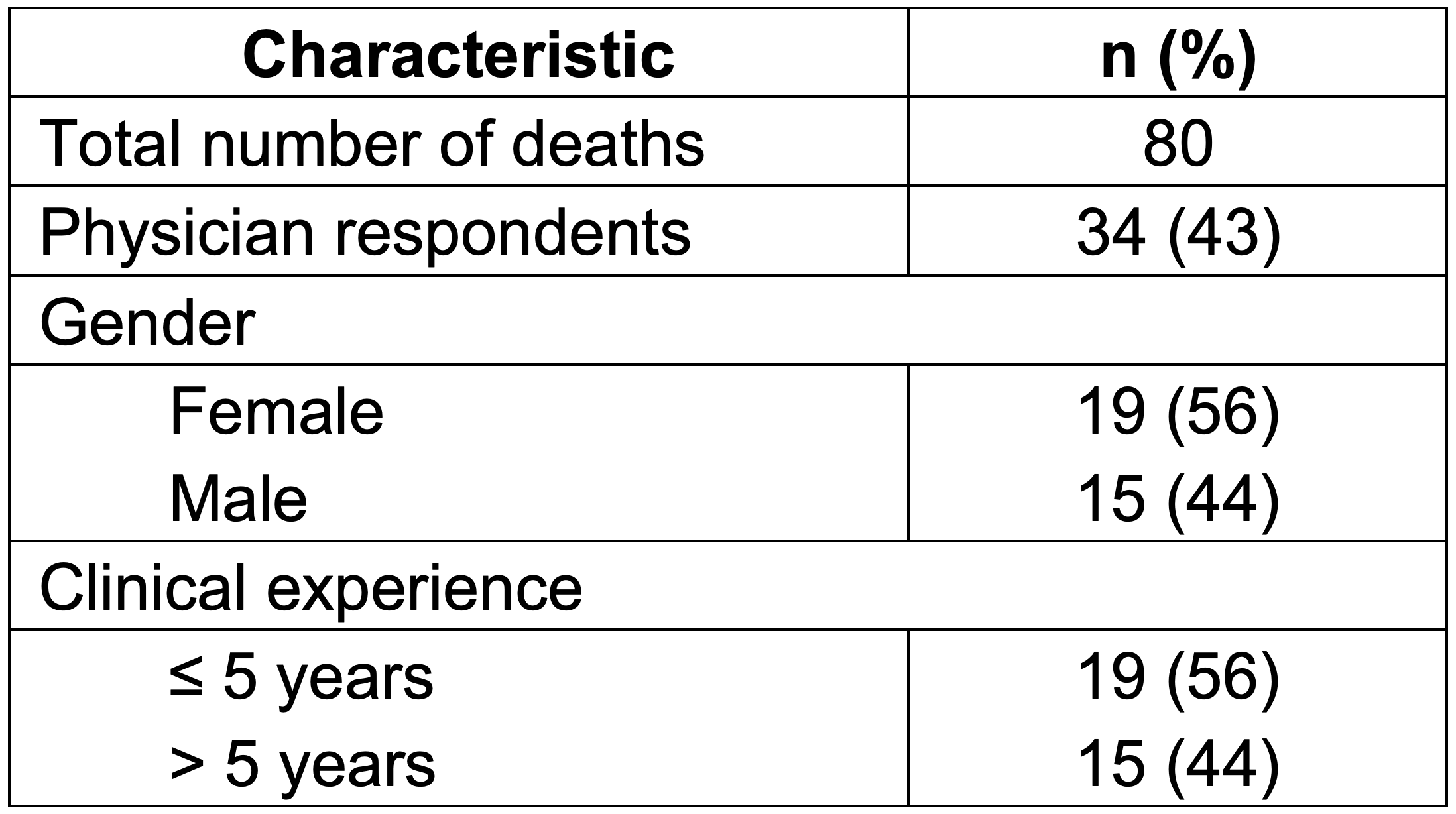
Figure 1 Current Review Process Following the Death of a Child