Infectious Diseases 4: Improving antibiotic use
Session: Infectious Diseases 4: Improving antibiotic use
141 - Is empiric coverage for methicillin resistant Staphylococcus aureus needed for uncomplicated pediatric bone and joint infections?
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 141.5687
Joel Rose-Kamprath, Dell Children's Medical Center of Central Texas, Austin, TX, United States; Marisol Fernandez, University of Texas at Austin Dell Medical School, Austin, TX, United States; Alec Wesolowski, Dell Children's Medical Center of Central Texas, Austin, TX, United States; Nyle Maissen, Dell Children's Medical Center of Central Texas, Austin, TX, United States; Rachel Downey, Dell Children's Medical Center of Central Texas, Autsin, TX, United States

Joel Rose-Kamprath, MS, MD
Resident Physician
Dell Children's Medical Center of Central Texas
Austin, Texas, United States
Presenting Author(s)
Background: Staphylococcus aureus, including those that are methicillin resistant (MRSA) is an important etiology of pediatric bone and joint infections (BJI). The prevalence of MRSA associated BJIs is declining nationally. This is likely multifactorial, attributed to improved infection control measures, antibiotic stewardship programs, and changes in virulence factors. Studies have also shown a rising resistance to clindamycin. Our institution’s current BJI guideline recommends empiric clindamycin for MRSA coverage in addition to a beta-lactam antibiotic. Rising resistance to clindamycin among Staphylococcus aureus isolates along with a decline in MRSA-caused infections locally and nationally calls into question the utility of empiric clindamycin.
Objective: Determine the local incidence of MRSA BJIs
Evaluate the need for empiric MRSA coverage in pediatric BJIs
Design/Methods: This single-center, multi-site, retrospective cohort study included pediatric patients admitted between January 2019 and April 2024 in Central Texas who were diagnosed with a BJI. Those with immunocompromised status, chronic osteomyelitis, post-surgical osteomyelitis or older than 18 years were excluded. Patient demographics, organisms isolated, antibiotic susceptibility, initial and final antibiotic regimens were extracted from the charts. Outcomes assessed included 30-day readmission, microbiologic failure, and relapse.
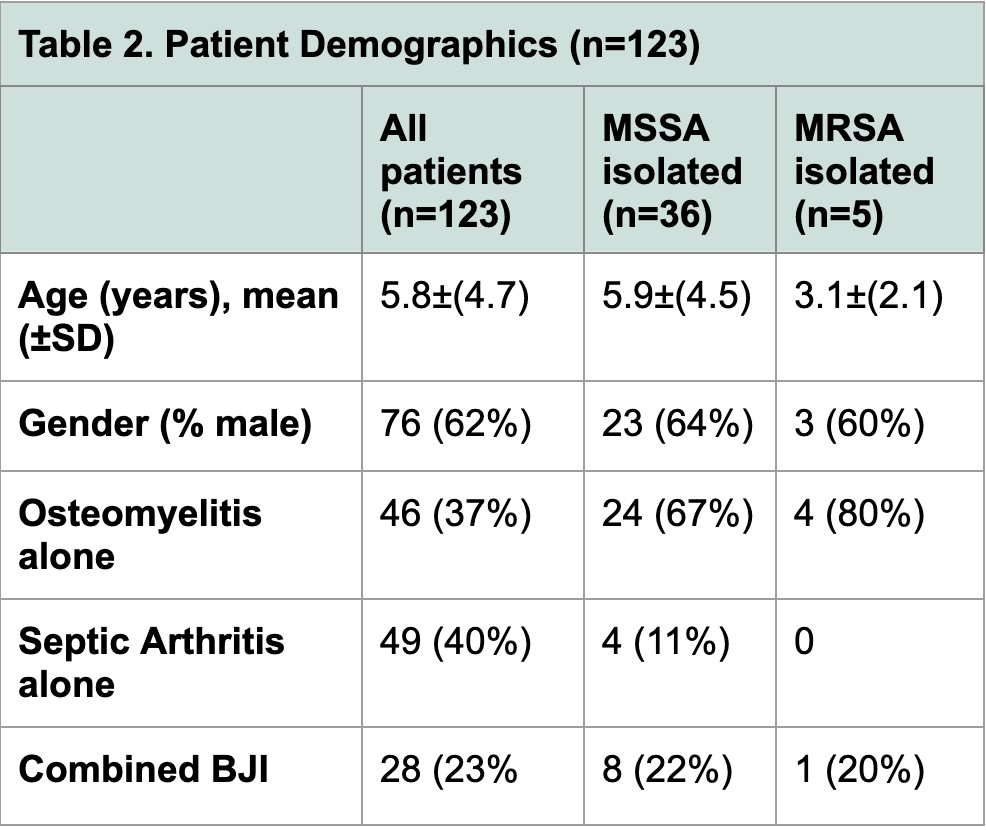
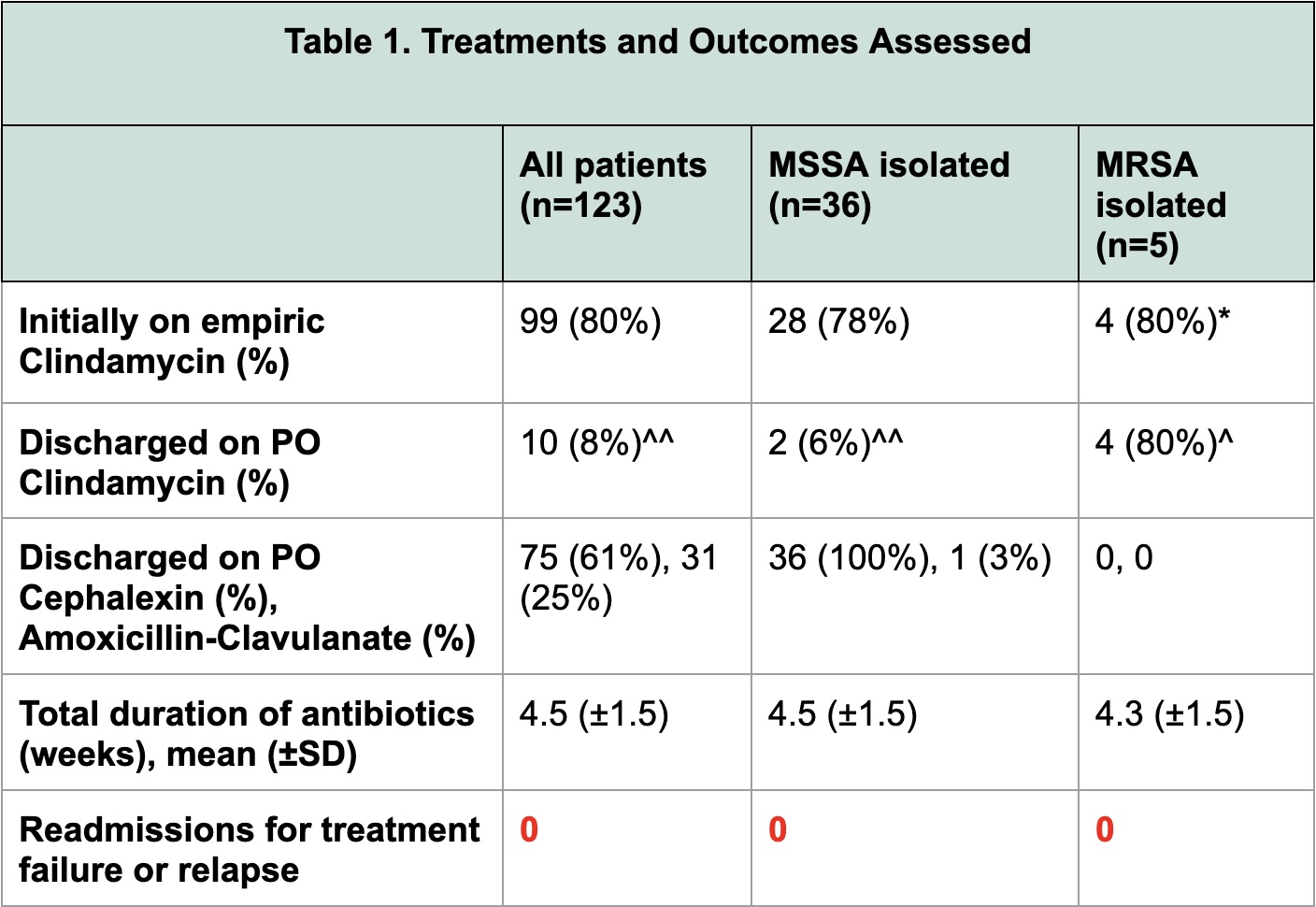
Results: 168 patient charts were reviewed and 123 patients were included. Table 1 summarizes patient demographics and distribution of BJIs. A bacterial pathogen was identified in 78 (63%) of cases. S. aureus was the most common pathogen identified in 41 (33%) cases; 5 (4%) cases were identified as MRSA. 99 (80%) patients received empiric clindamycin. Among the 45 cases without a pathogen identified, 37 (82%) were empirically started on MRSA coverage with clindamycin; 41 (91%) were discharged without antibiotics against MRSA. There were no readmissions for treatment failure or relapse across all patients included. Table 2 summarizes the treatments and outcomes assessed for the patients included.
Conclusion(s): Our review of 5 years of data on BJIs in Central Texas revealed a low rate of confirmed MRSA (4%). In this sample, 86% of cases were discharged without MRSA coverage, including those without a pathogen identified. None required readmission for treatment failure or relapse. The need for empiric MRSA treatment in cases of uncomplicated BJI might not be necessary in areas of low MRSA prevalence.
Table 1. Treatments and Outcomes Assessed
 *One patient was initially on Vancomycin
*One patient was initially on Vancomycin^One patient completed full antibiotic course inpatient
^^Two patients developed rash with Cephalexin and were switched to Clindamycin
Table 2. Patient Demographics (n=123)