Health Equity/Social Determinants of Health 2
Session: Health Equity/Social Determinants of Health 2
421 - Neighborhood Socioeconomic and Geographic Determinants of Prenatal Congenital Heart Disease Diagnosis
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 421.5754
Matthew M. Tran, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Mary D. Schiff, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Floyd W. Thoma, UPMC Heart and Vascular Institute, Pittsburgh, PA, United States; Frederick W.. Roberts, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Craig P. Dobson, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States

Matthew M. Tran, MD
Fellow Physician
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Prenatal detection of congenital heart disease (CHD) has been shown to decrease neonatal morbidity and mortality. It is known that there is a disparity in fetal echocardiography in women in lower socioeconomic quartiles (SEQ), who live in rural residences, types of insurance, race, and ethnicity.
Objective: To determine if aspects of the neighborhood social, economic, and urban/rural location contribute to disparities in prenatal CHD detection in Western Pennsylvania.
Design/Methods: The retrospective single center study evaluated infants < 6 months of age with neonatal CHD requiring surgical intervention (excluding only patent ductus arteriosus ligation) between 2010 and 2024. Infants were identified through the Society of Thoracic Surgeons (STS) database and ICD-9 and ICD-10 codes for major CHD and surgeries. The infant was linked to the mother to establish a dyad, and billing data was used to determine whether the mother had a fetal echocardiogram within 6 months of birth. Characteristics, including Area Deprivation Index (ADI), rurality, and walkability, were compared between prenatal CHD diagnosis groups using Wilcoxon-Mann-Whitney tests, and chi-square or Fisher’s exact tests. Odds ratios (OR) and 95% confidence intervals (CI) were obtained from multi-level logistic regression models assessing the association between each neighborhood predictor and having a prenatal CHD diagnosis.
Results: 442 (52%) of the 847 mother-infant dyads had a prenatal CHD diagnosis. Those with a prenatal diagnosis were more likely to live in communities of high neighborhood socioeconomic deprivation (p=0.0011), and were more likely to be Black (p=0.0102). Those living in the most deprived communities had the highest rate of prenatal diagnosis (61%) compared to those living in moderately deprived (47%) and low deprivation (49%) neighborhoods (p=0.0011). CHD was not more prevalent in higher deprivation communities. Patients who lived in the most socioeconomically deprived communities had 55% greater odds of having a prenatal CHD diagnosis (p=0.0157) compared to patients who lived in the most socioeconomically advantaged communities. Moreover, each 10-point increase in the ADI was associated with 7% greater odds of having a prenatal CHD diagnosis (p=0.0387). Neither rurality, neighborhood walkability, nor insurance type were associated with prenatal diagnosis.
Conclusion(s): Surprisingly, the prenatal detection rate is higher in more deprived communications, and the rate was higher in Black mothers. There was no significant effect of rurality, walkability, or insurance type on prenatal detection of CHD.
Table 1. Description of sample characteristics, overall and by missed prenatal diagnosis status in sample (n=847 patients).
.png) Data are reported as n (%), mean sd, or median (1st, 3rd quartiles). ADI score ranges from 0-100, with higher scores indicating more neighborhood socioeconomic disadvantage. Walk-Score ranges from 0-100, with higher scores indicating more walkable environments. ADI = Area Deprivation Index, CHD = congenital heart disease.
Data are reported as n (%), mean sd, or median (1st, 3rd quartiles). ADI score ranges from 0-100, with higher scores indicating more neighborhood socioeconomic disadvantage. Walk-Score ranges from 0-100, with higher scores indicating more walkable environments. ADI = Area Deprivation Index, CHD = congenital heart disease. Table 2. Association between neighborhood socioeconomic deprivation tertile and having a prenatal CHD diagnosis.
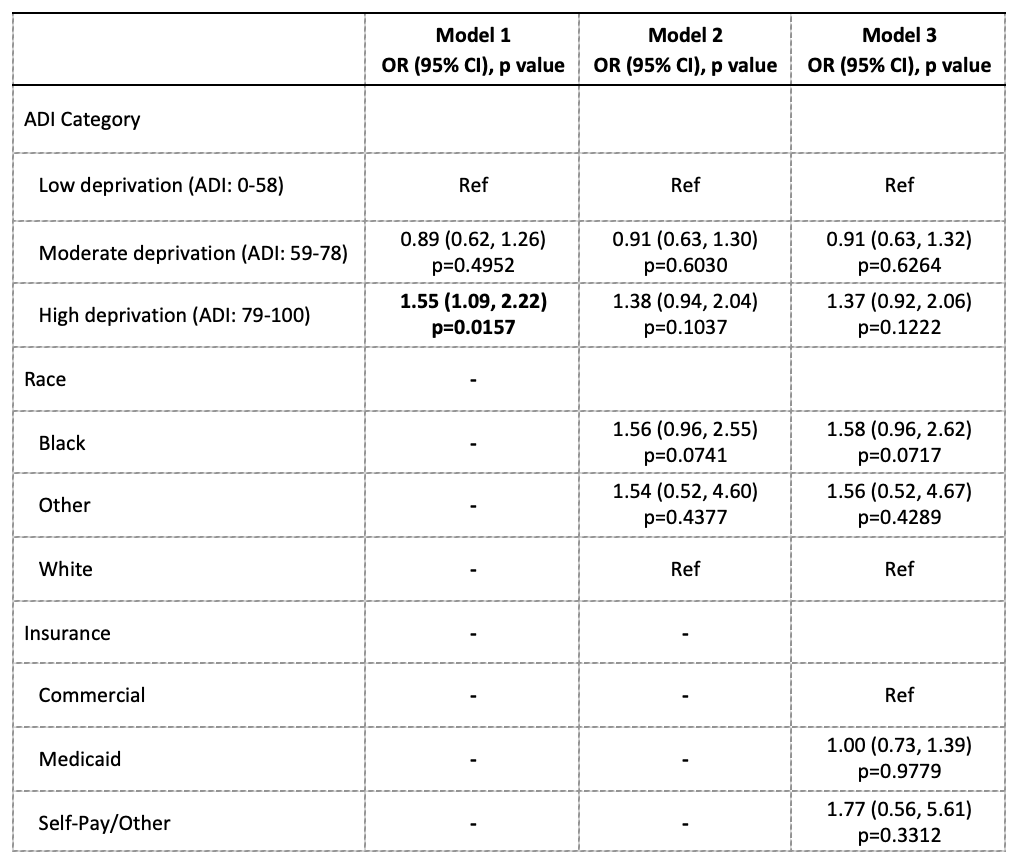 Effects estimated from multi-level logistic regression models, with a random intercept term included to account for patients nested within zip codes. Model 1 is unadjusted for covariates. Model 2 is adjusted for race. Model 3 is adjusted for Model 2 + insurance type. Bolded estimates indicate statistical significance at the 0.05 alpha level. ADI, Area Deprivation Index score ranges from 0-100, with higher scores indicating more neighborhood socioeconomic disadvantage; OR, odds ratio; CI, confidence interval; CHD, congenital heart disease.
Effects estimated from multi-level logistic regression models, with a random intercept term included to account for patients nested within zip codes. Model 1 is unadjusted for covariates. Model 2 is adjusted for race. Model 3 is adjusted for Model 2 + insurance type. Bolded estimates indicate statistical significance at the 0.05 alpha level. ADI, Area Deprivation Index score ranges from 0-100, with higher scores indicating more neighborhood socioeconomic disadvantage; OR, odds ratio; CI, confidence interval; CHD, congenital heart disease. Table 3. Association between neighborhood socioeconomic deprivation score and having a prenatal CHD diagnosis.
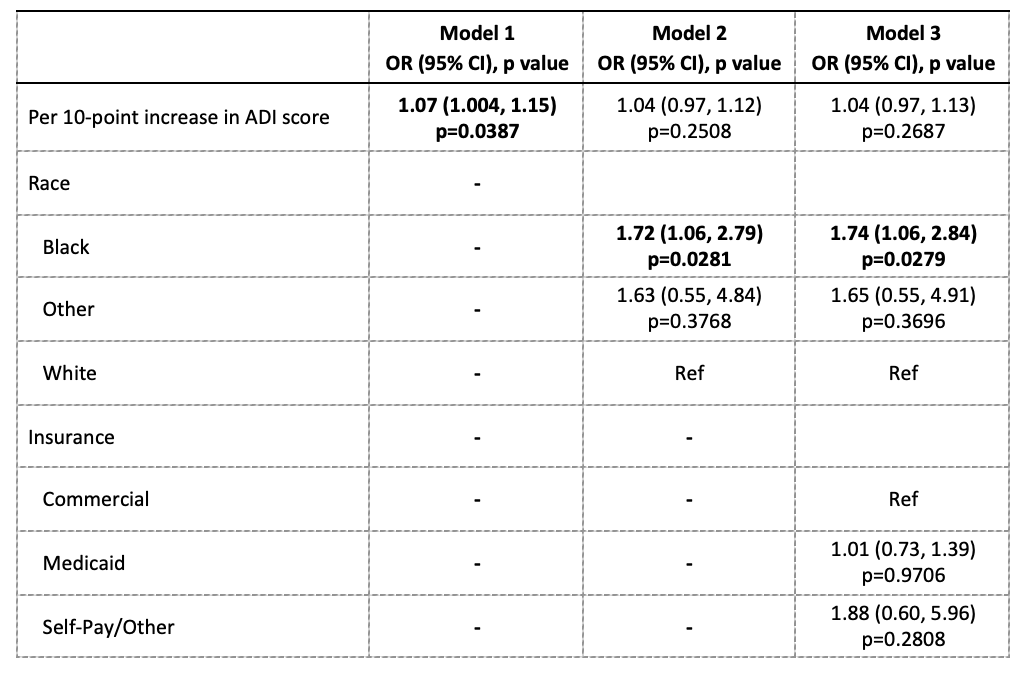 Effects estimated from multi-level logistic regression models, with a random intercept term included to account for patients nested within zip codes. Model 1 is unadjusted for covariates. Model 2 is adjusted for race. Model 3 is adjusted for Model 2 + insurance type. Bolded estimates indicate statistical significance at the 0.05 alpha level. ADI, Area Deprivation Index score ranges from 0-100, with higher scores indicating more neighborhood socioeconomic disadvantage; OR, odds ratio; CI, confidence interval; CHD, congenital heart disease.
Effects estimated from multi-level logistic regression models, with a random intercept term included to account for patients nested within zip codes. Model 1 is unadjusted for covariates. Model 2 is adjusted for race. Model 3 is adjusted for Model 2 + insurance type. Bolded estimates indicate statistical significance at the 0.05 alpha level. ADI, Area Deprivation Index score ranges from 0-100, with higher scores indicating more neighborhood socioeconomic disadvantage; OR, odds ratio; CI, confidence interval; CHD, congenital heart disease.
