Mental Health 1
Session: Mental Health 1
757 - Impact of an interdisciplinary, peer-led clinical mental health education intervention on pediatrics trainee comfort with outpatient mental health concerns
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 757.5230
Kristen M. Durbin, University of Utah School of Medicine, Salt Lake City, UT, United States; Joni Hemond, University of Utah School of Medicine, Salt Lake City, UT, United States

Kristen M. Durbin, MD (she/her/hers)
Assistant Professor
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: The prevalence of youth mental illness in Utah is more than 20 percent; however, with 6 child psychiatrists per 100,000 children, the state workforce does not meet patient needs. Although pediatricians often provide mental health care for children, 65% of those surveyed nationally by the American Academy of Pediatrics in 2013 felt underprepared to do so. Triple Board (TB; pediatrics, adult psychiatry, child/adolescent psychiatry) trainees are uniquely suited to strengthen the local mental health workforce by educating pediatrics trainees within a clinical mental health integration (MHI) model.
Objective: To assess the impact of peer-led MHI education on pediatrics trainee comfort with diagnosis and treatment of common mental health concerns.
Design/Methods: An optional, anonymous survey gauged AY 2023-24 pediatrics trainee baseline comfort with diagnosis and treatment of attention deficit-hyperactivity disorder (ADHD), depression, anxiety, behavior disorders, autism spectrum disorder (ASD), and trauma. Trainees participated in MHI education, in which TB residents led an Intro to MHI lecture, shadowing visits, and small group teaching. A post-survey was administered with request for feedback on the education intervention. Pre- and post-survey data were analyzed with unpaired t-tests.
Results: Initial trainee survey response was n=29; follow up response was n=18. Respondents reported higher baseline mean comfort with mental health diagnosis than with treatment; they had more comfort with ADHD, depression, and anxiety than with behavior disorders, ASD, and trauma. At follow-up, respondents reported improved comfort with both diagnosis and treatment of all six mental health concerns, with statistically significant change in comfort level noted in all domains (p < 0.05). See tables 1-3. Pertinent themes from comments on the education intervention include: benefit of working clinically with TB residents; benefit of didactic teaching; improved understanding of MHI model.
Conclusion(s): Implementing an interdisciplinary, peer-led clinical mental health education intervention is an effective strategy to improve pediatrics trainee comfort with outpatient mental health concerns. Continued trainee clinical practice between surveys is a confounder, but trainee comments indicate the education intervention was impactful. Additional trainee education is warranted for behavior disorders, ASD and trauma. Although this study was limited in size, our data indicate that other institutions may benefit from developing peer-led clinical mental health education curricula for trainees.
Comfort with Diagnosis of Mental Health Concerns
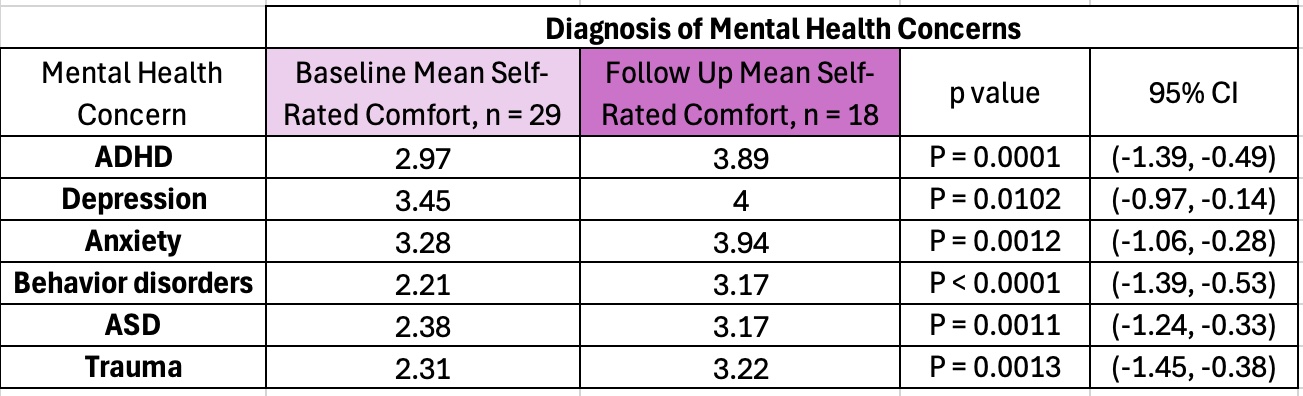 Note: Comfort was self-reported on a 1-5 Likert scale from “Not at all comfortable” to “Very comfortable” for each of six mental health concerns, with separate ratings for comfort with diagnosis and treatment of each concern (Tables 1 and 2, respectively)
Note: Comfort was self-reported on a 1-5 Likert scale from “Not at all comfortable” to “Very comfortable” for each of six mental health concerns, with separate ratings for comfort with diagnosis and treatment of each concern (Tables 1 and 2, respectively)Comfort with Treatment of Mental Health Concerns
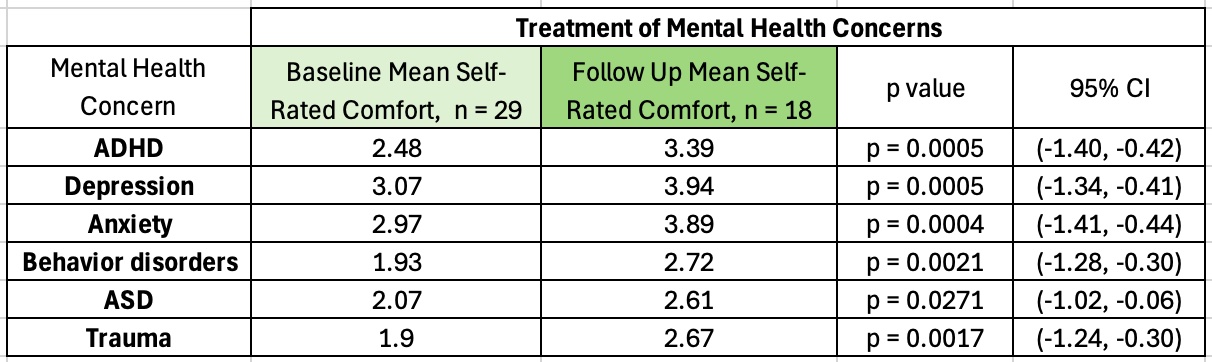 Note: Comfort was self-reported on a 1-5 Likert scale from “Not at all comfortable” to “Very comfortable” for each of six mental health concerns, with separate ratings for comfort with diagnosis and treatment of each concern (Tables 1 and 2, respectively)
Note: Comfort was self-reported on a 1-5 Likert scale from “Not at all comfortable” to “Very comfortable” for each of six mental health concerns, with separate ratings for comfort with diagnosis and treatment of each concern (Tables 1 and 2, respectively)Mean Trainee Comfort with Mental Health Diagnosis and Treatment, Baseline vs. Follow Up - AY 2023-2024
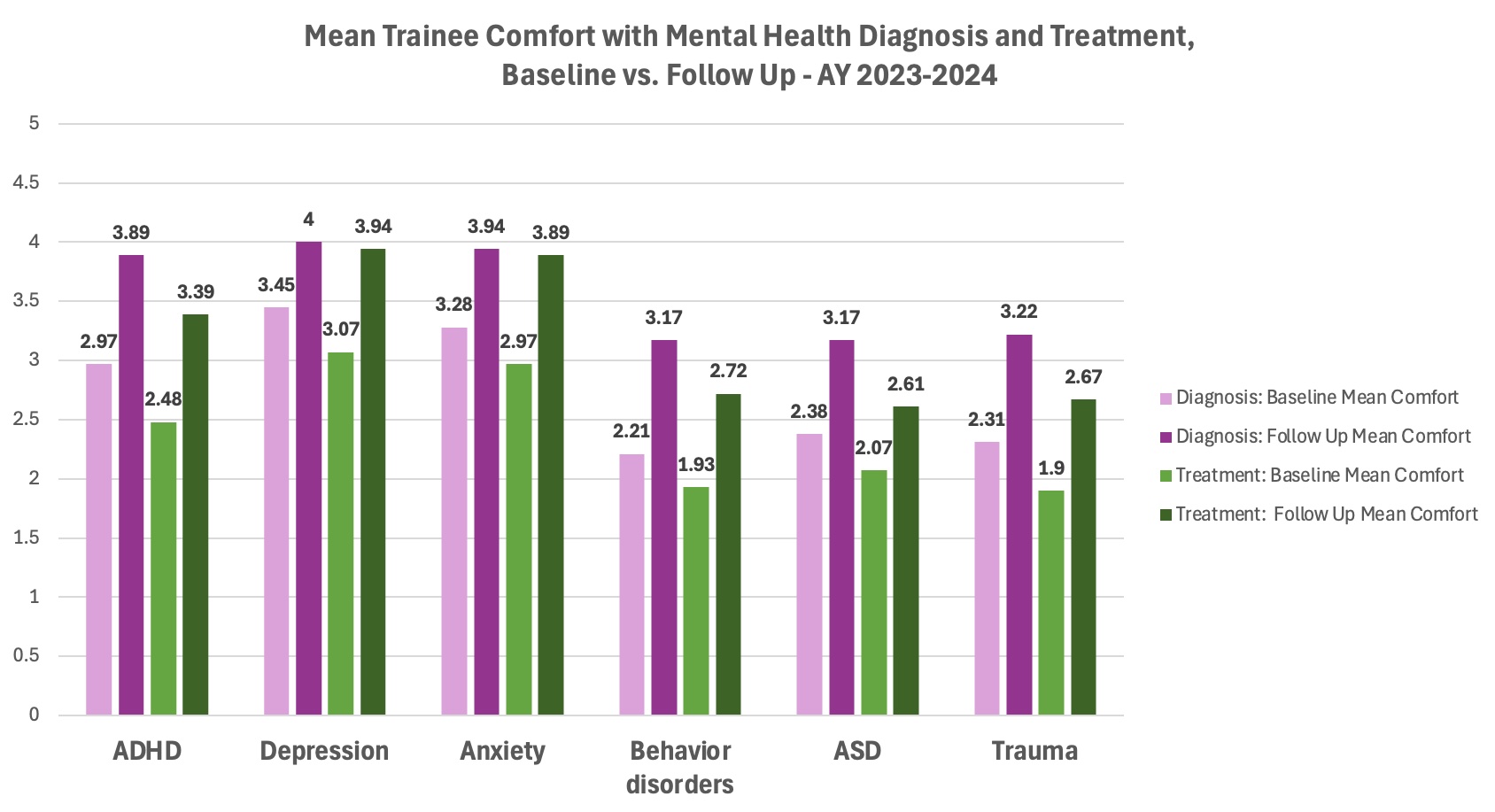 Rated on Likert scale 1-5
Rated on Likert scale 1-5
