Hospital Medicine 1: Quality Improvement
Session: Hospital Medicine 1: Quality Improvement
550 - Improving a Situation Awareness Model to Allow Early Identification of Patients at Risk of Clinical Deterioration
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 550.5268
Olivia Post, Cincinnati Children's Hospital Medical Center, Loveland, OH, United States; Michelle Coleman, Cincinnati Children's Hospital and Medical Center, Cincinnati, OH, United States; Katy Bedinghaus, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Jennifer L. Carmichael, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Brittany L. Frakes, CCHMC, Villa Hills/Crescent Springs/Ft. Mitchell, KY, United States; Rae Becker, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Laura R. Hatcher, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, OH, United States; Erin Molloy, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Laura Brower, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States

Olivia Post, MD (she/her/hers)
Hospital Medicine Clinical Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Pediatric patients who require emergency transfer (ET) to a critical care unit have worse outcomes, longer length of stay (LOS) post-transfer, and higher in-hospital mortality than matched controls. An ET is a floor to ICU transfer in which one of the following interventions occurs within 1 hour of transfer: intubation, receipt of inotropes, or at least 60 mL/kg of fluid resuscitation (including blood products). Previous implementation of a situation awareness model that identified and addressed risk factors for clinical deterioration reduced the rate of ETs in our hospital. After this initial reduction period, we experienced a sustained increase in the rate of ETs, prompting us to focus on opportunities for earlier utilization of the model.
Objective: To increase the percentage of acute care patients who are identified as watchers prior to activation of a medical response team (MRT) or code to decrease the rate of ETs.
Design/Methods: We identified key drivers including appropriate assessment of the patient with an ability to detect changes in clinical status, early identification of patients at risk of deterioration, a standardized clinical pathway for escalation of concern with usable tools, and psychological safety to escalate concerns and ask questions (Figure 1). We iteratively implemented PDSA cycles including the creation of unit-specific automatic watcher criteria, situation awareness education for nursing team members, and the creation of an escalation pathway (Figure 2). A critical care outreach team was also implemented by the ICU team in 2022. Our primary process measure was the percentage of patients identified as watchers prior to MRT or code. Our secondary outcome measure was the number of ETs per 10,000 patient days. We used run charts to determine center-line shifts.
Results: The percentage of patients identified as watchers prior to activation of MRT or code increased from 41% to 47.6% from 2022 to the end of fiscal year 2024 (Figure 2). The number of ETs remained relatively stable at 2.85 events per 10,000 patient days in 2024 compared to 3.5 in 2022.
Conclusion(s): We successfully increased the percentage of patients identified as watchers prior to MRT or code through implementation of various tools to allow earlier detection of clinical deterioration as well as a standardized escalation pathway. Despite this, the number of ETs remained largely unchanged. Future directions will focus on re-evaluation of other factors contributing to the key drivers.
Figure 1.
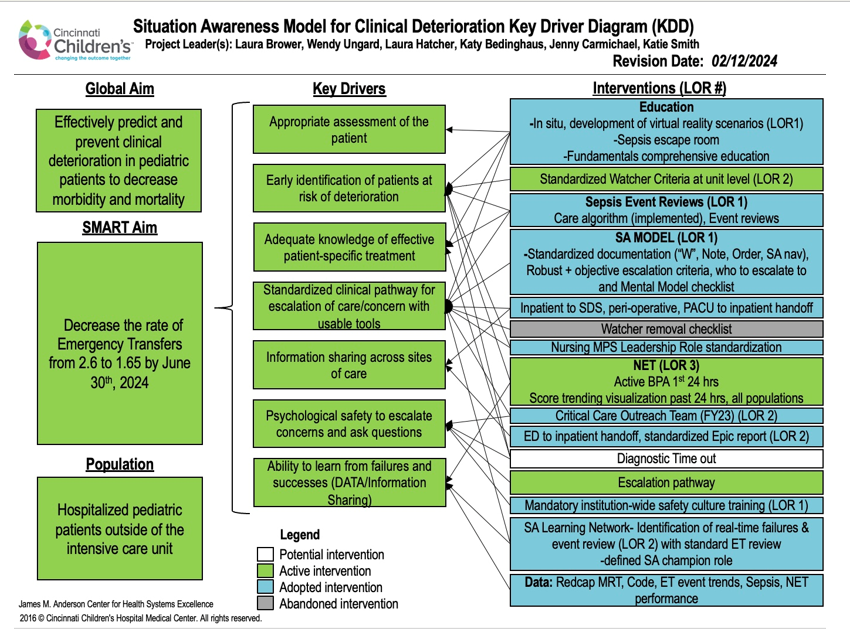 Key driver diagram for situation awareness model.
Key driver diagram for situation awareness model. Figure 2.
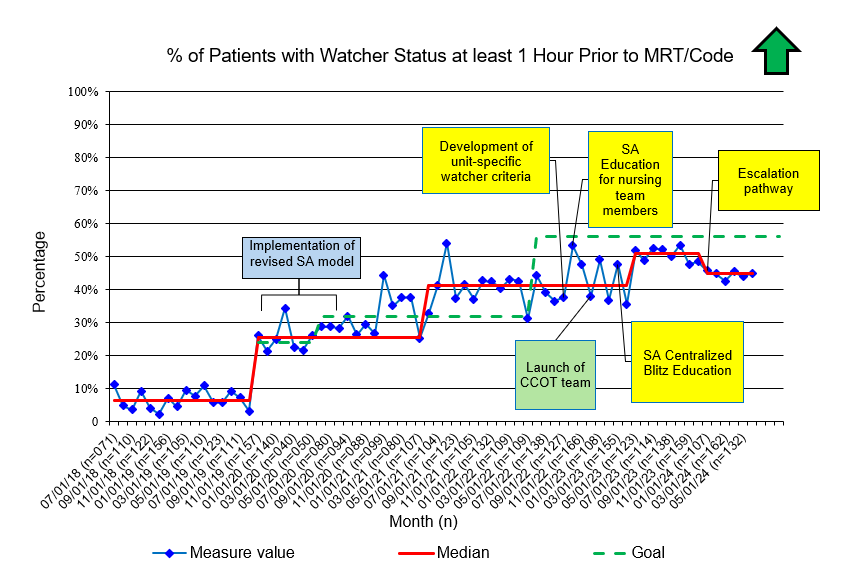 Run chart detailing percentage of patients with watcher status at least one hour prior to MRT or code. Interventions by situation awareness team are in yellow. Other institutional interventions which may have impacted the primary process measure are in green.
Run chart detailing percentage of patients with watcher status at least one hour prior to MRT or code. Interventions by situation awareness team are in yellow. Other institutional interventions which may have impacted the primary process measure are in green. 

