Quality Improvement/Patient Safety 6
Session: Quality Improvement/Patient Safety 6
488 - Improving operating room throughput inefficiencies using advanced improvement science methods and factorial design
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 488.5247
John M. Harris, CHOC Children's Hospital of Orange County, Orange, CA, United States; Jennifer Combs, CHOC Children's Hospital of Orange County, Irvine, CA, United States; Sandip A.. Godambe, CHOC Children's Hospital of Orange County, Orange, CA, United States

John M. Harris, MD (he/him/his)
Executive Director Surgical Services
CHOC Children's Hospital of Orange County
Orange, California, United States
Presenting Author(s)
Background: Delays in operating room FCOTS (First Case On Time Starts) can lead to a cascade of deleterious effects including increased waste, operational costs, patient harm, staff culture burnout, and family dissatisfaction. Post-COVID our surgical services saw a decline in FCOTS to 76%.
Objective: To establish interventions which improve FCOTS and efficiencies in the operating theatre.
Design/Methods: This QI project occurred at an urban children’s hospital using a multidisciplinary improvement-team, the Model for Improvement (MFI) and factorial design. We developed multiple tests of change to identify effective factors, namely communication techniques. Using factorial design, the inter-relationships between the different factors were determined and which was the most effective at reducing FCOTS.
Results: A Pareto analysis of delays in FCOTS in the operating theatre identified late arrivals by surgeons and anesthesiologists as the most frequent contributing factors. The first interventions utilized were texting reminders to these two teams which resulted in improving FCOTS from 72% to 88% and decreasing the average time delayed from 7.49 min to 4.22 min (Fig 1). Statistical process control analysis of the FCOTS between December 2022 and June 2023 indicated these improvements were not sustained, with the average delays per case increasing to 5.42 minutes late per case compared to the previous 4.22 minutes.
A 2X2 factorial planned experiment was initiated as Phase Two between December 2022 and August 2023. The first case start times improved from 5.42 to 4.41 avg min late (Fig 2). Factorial analysis (Fig 3) showed that single notification of either the anesthesiologist or surgeon was more effective than notification of both. The room Turn Around Times (TAT) improved from 21.07 to 18.96 min, a 10% reduction.
Conclusion(s): FCOTS and TAT are key metrics for evaluating operating room efficiency and performance. Through the application of the MFI and factorial design, significant improvements were achieved by introducing targeted interventions, including evening text reminders to specific services, the formation of multidisciplinary improvement teams, and fostering a stronger culture of communication. This is evident by a 22% improvement in percent FCOTS, a 41% reduction in avg min late per case, an overall improvement in TAT of 10%, and a soft net revenue savings of $5,000,000. Optimally performing systems, when not overburdened, promote consistent reproducible care with less variability, enhanced patient safety and overall operational reliability.
Phase One Average Delay in Minutes by Stage
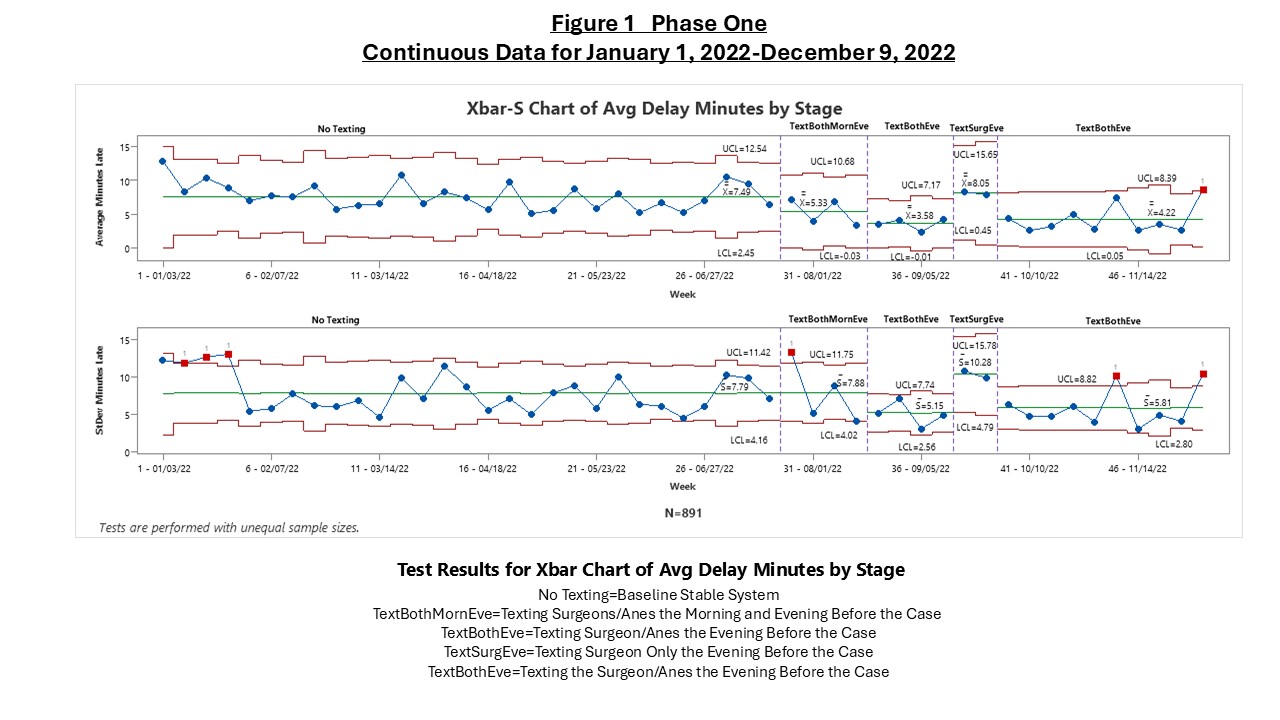 This is an Xbar-S chart that shows the results of the different stages reflecting different interventions.
This is an Xbar-S chart that shows the results of the different stages reflecting different interventions. Phase Two Average Delay in Minutes by Stage
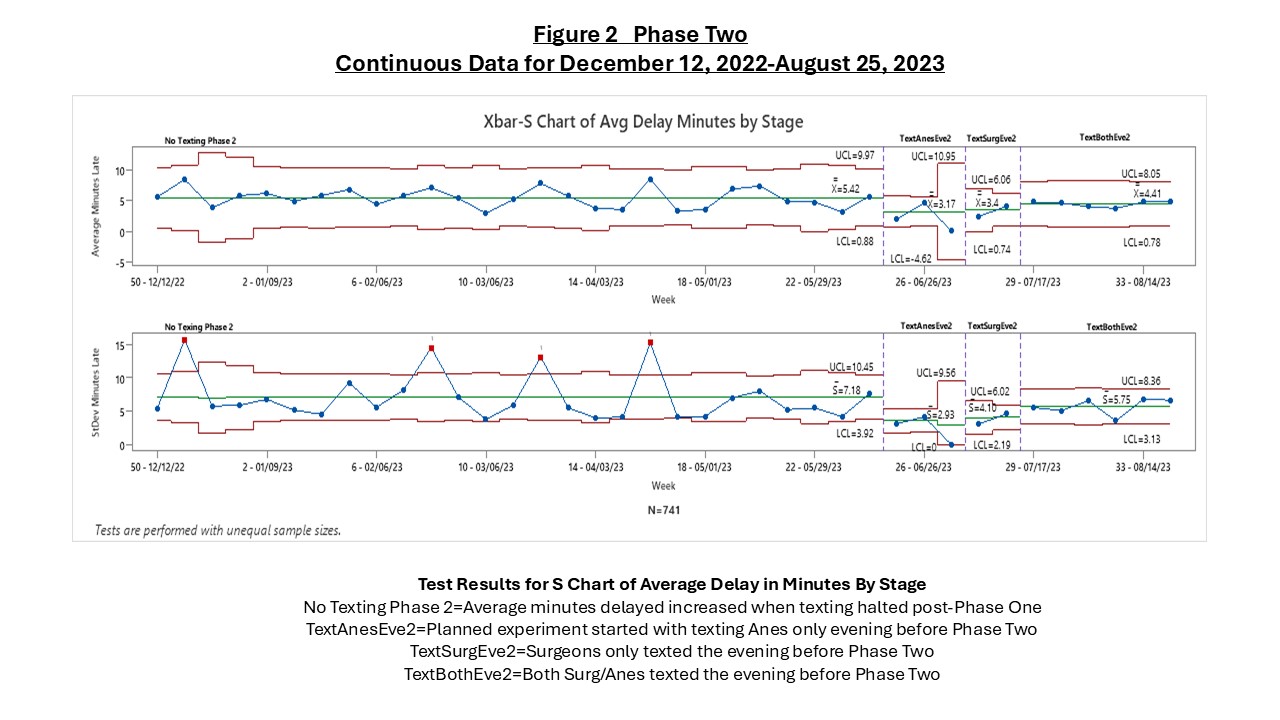 This is an Xbar-S chart that shows the results of the different stages reflecting different interventions.
This is an Xbar-S chart that shows the results of the different stages reflecting different interventions. Planned Experiment or Factorial Design Demonstrating the Effects on the Different Texting Strategies on Operative Start Time
.jpg) The Dot Diagram shows the effects of the different texting strategies on the first case start times. "A" reflects when only the Anesthesiologist was texted, "S" when only the Surgeon was texted, and "AS" reflects when both the Anesthesiologist and Surgeon were texted. The response plots to the right shows the relationship for each of the three combinations of two factors, where "ATR" represents Anesthesia Text Reminder and "STR" represents Surgeon Text Reminder.
The Dot Diagram shows the effects of the different texting strategies on the first case start times. "A" reflects when only the Anesthesiologist was texted, "S" when only the Surgeon was texted, and "AS" reflects when both the Anesthesiologist and Surgeon were texted. The response plots to the right shows the relationship for each of the three combinations of two factors, where "ATR" represents Anesthesia Text Reminder and "STR" represents Surgeon Text Reminder.

