Neonatal Hemodynamics and Cardiovascular Medicine 2
Session: Neonatal Hemodynamics and Cardiovascular Medicine 2
054 - Inhaled nitric oxide in very low birth weight infants; A single centre retrospective chart review
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 54.5430
Robert Joyce, Cork University Maternity Hospital, Dublin, Dublin, Ireland; Chiara Passarella, Ospedale Pediatrico Bambino Gesù, Laveno Mombello, Lombardia, Italy; Vicki Livingstone, University College Cork, Cork, Cork, Ireland; Brian Walsh, Infant Centre, University College Cork, Cork, Cork, Ireland; Eugene M. Dempsey, University College Cork, Cork, Cork, Ireland

Robert Joyce, MRCPI MB BCh BAO
Neonatal Specialist Registrar
Cork University Maternity Hospital
Dublin, Dublin, Ireland
Presenting Author(s)
Background: Inhaled nitric oxide (iNO) is a potent pulmonary vasodilator well established in the treatment of term infants with persistent pulmonary hypertension of the newborn (PPHN). While it is often used in the treatment of very low birthweight (VLBW) infants with respiratory failure, it’s efficacy has not been shown in this population.
Objective: Determine the effect of iNO on ventilatory requirements in the 4 hours following initiation of treatment in VLBW with respiratory failure. Secondary outcomes included echocardiogram indices of PPHN pre and post-iNO initiation, and clinical outcomes in VLBW infants treated with iNO.
Design/Methods: A retrospective study of infants born weighing less than 1500g treated with iNO at our institution over the past 7 years (2017-2023). We reviewed the charts of infants reported to the Vermont Oxford Network (VON), as well as electronically stored echocardiograms of infants who received iNO (5 days prior to iNO initiation or within 3 days of initiation). Oxygen saturation index (OSI) was calculated for each infant at treatment initiation, and 4 hours post.
Results: A total of 576 VLBW infants were born at Cork University Maternity Hospital (Cork, Ireland). Of these, 58 (10.1%) received iNO. The population treated with iNO were smaller, more premature, had worse APGARS, and were more likely to have a histological diagnosis of chorioamnionitis than those not treated with iNO (all p< 0.001). The mortality rate for these infants was 62%, compared to 8.3% in those not treated with iNO. There was a significant correlation between iNO use and multiple complications of prematurity (Table 1).The most common aetiology of hypoxic respiratory failure treated with iNO was PPHN/pulmonary hypoplasia at 24/58 (41.4%), followed by respiratory distress syndrome (RDS)/pulmonary interstitial emphysema (PIE) at 13/58 (22.4%).
Echocardiograms were available in 36/58 (62.1%), with features of PPHN present in 31/36 (86.1%). There was a clinical and/or echocardiographic diagnosis of PPHN in 42/58 (72.4%). A valid OSI could be determined in 57/58 cases. Median OSI was 12.6 (IQR 10.2, 16.9) at treatment initiation. iNO use was associated with a significant improvement in OSI after 4 hours of treatment (median 10.3 [5.7, 14.8]).
Conclusion(s): iNO use in our population of VLBW infants was associated with a significant improvement in OSI within 4 hours of commencement. However these OSI scores were consistent with severe hypoxic respiratory failure at treatment initiation, reflected in poor outcomes as a cohort. iNO use is associated with a significant increase in mortality or BPD in survivors.
Table 1
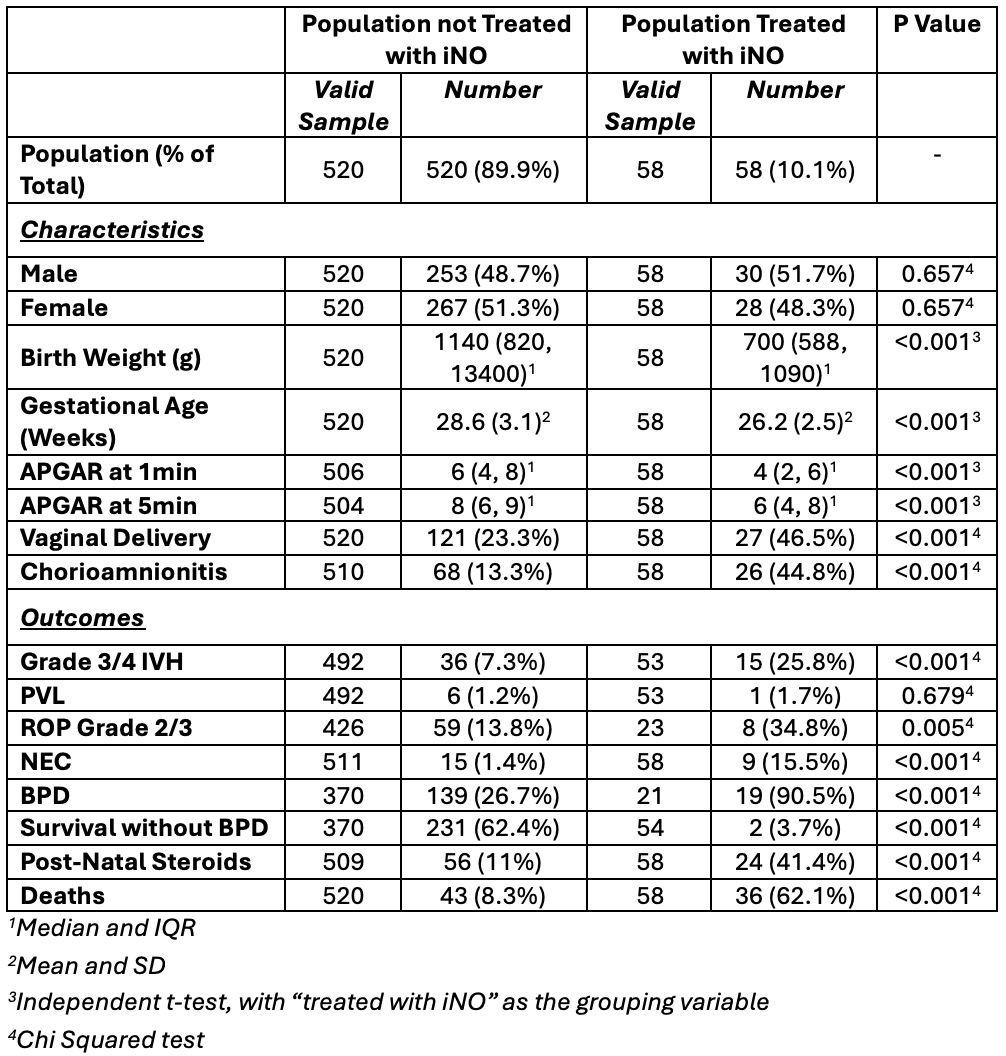 Population Comparisons
Population ComparisonsTable 2
.png) Pre and Post-iNO Initiation Respiratory Parameters
Pre and Post-iNO Initiation Respiratory ParametersTable 3
.png) OSI Change by Characteristic
OSI Change by Characteristic
