Hospital Medicine 2: Quality Improvement
Session: Hospital Medicine 2: Quality Improvement
564 - Improving Utilization of Disease Specific Order Sets on Admission in Hospitalized Children
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 564.5425
Elena Dingle, Akron Children's Hospital, Cuyahoga Falls, OH, United States; Karen C. Willis, Akron Children's Hospital, Akron, OH, United States; Erin Pitchure, Akron Children's Hospital, Akron, OH, United States; Samantha Gunkelman, Akron Children's Hospital, Akron, OH, United States

Elena Dingle, MD, PhD, FAAP (she/her/hers)
PHM fellow
Akron Children's Hospital
Cuyahoga Falls, Ohio, United States
Presenting Author(s)
Background: Implementing order sets has proven to be an effective strategy for delivering standardized, evidence-based care, helping to keep medical practices current and economically efficient. Studies have shown that using disease-specific order sets (DSOS) is linked to decreased lengths of stay, a reduction in unnecessary respiratory treatments, and lower hospital costs for certain pediatric conditions, including asthma and bronchiolitis. However, utilization of DSOS is not as high as it could be to provide benefits to patient care and the literature is limited on the use of DSOS in hospitalized children.
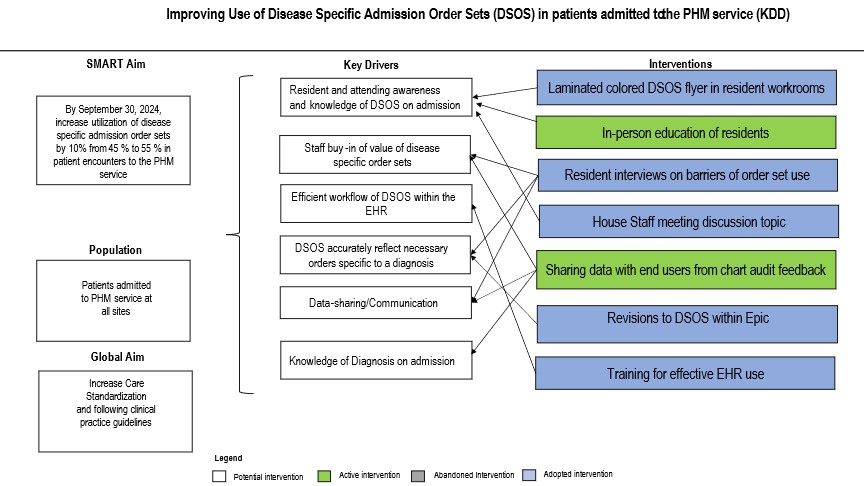
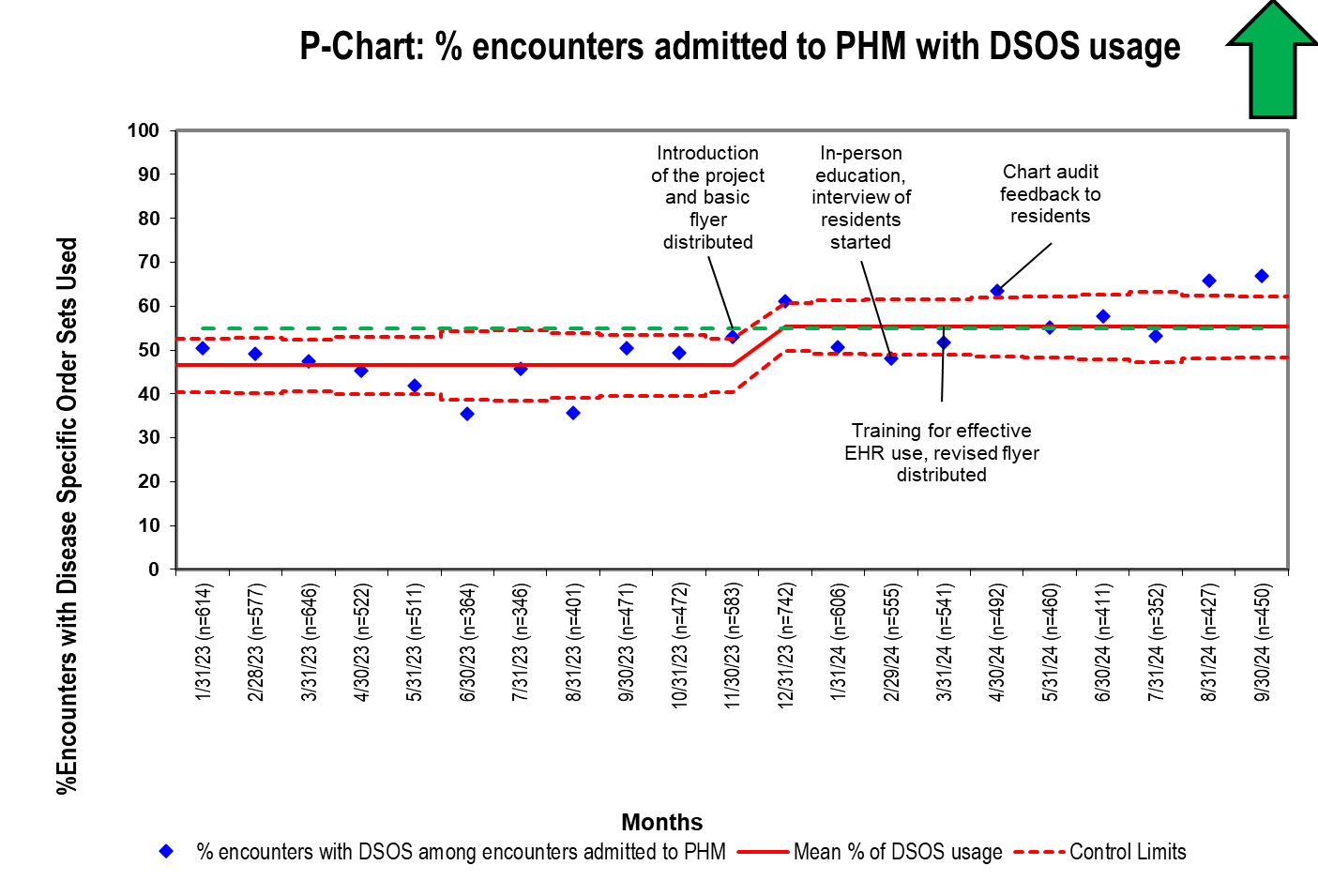
Objective: To increase the percentage of encounters with DSOS usage on admission to a Pediatric Hospital Medicine (PHM) service by 10% from 45% to 55% by September 30, 2024. Prior to the start of the project, the general inpatient admission order set (GIAOS) was commonly utilized for patients whose diagnoses had specific DSOS available. Therefore, a secondary objective was to reduce the percentage of encounters with GIAOS by 8%, from 53% to 45% by September 30, 2024.
Design/Methods: This project was conducted at a freestanding quaternary care children's hospital, specifically targeting patients admitted to PHM. A core team was formed composed of attendings, nurse practitioners, an electronic health record (EHR) support team member, a pediatric resident, and a PHM fellow. The Model for Improvement was used with key drivers being awareness of DSOS, buy-in of benefit of utilization, and efficient workflow. Key interventions included: in-person education of residents on DSOS, training for effective EHR use, laminated colored DSOS flyers, resident interviews on barriers to use of DSOS, chart audit feedback, revisions to DSOS within Epic. These interventions were tested and refined using plan-do-study-act (PDSA) cycles. Control charts were used to monitor data and inform the work process.
Results: During the improvement period, encounters with DSOS increased by 10%, from 45% to 55%. Additionally, there was a 9% decrease in the use of GIAOS, dropping from 53% to 44%. Our balancing measure indicated no safety events related to DSOS use were reported in the hospital's safety event reporting system.
Conclusion(s): The usage of DSOS among children admitted to PHM can be safely increased with interventions focusing on DSOS education, introduction of visual references and chart audit feedback to provide more standardized care.
KDD: Improving Use of Disease Specific Order Sets in Patients Admitted to the PHM Service
P-Chart: % of Encounters with DSOS Admitted to the PHM Service
P-Chart: % of Encounters Admitted to PHM with General Admission Order Set Usage
.png)


