Technology 2: Telemedicine
Session: Technology 2: Telemedicine
183 - Addition of a Dedicated Pediatric Telemedicine Provider in a Large Integrated Hospital System - Effects from a Pilot Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 183.3997
Sarah Becker, University of Utah School of Medicine, Salt Lake City, UT, United States; Howard Kadish, University of Utah School of Medicine, Salt Lake City, UT, United States; Amy Back, Primary Children's Hospital, SLC, UT, United States; Casey Bologna, Primary Children's Hospital, Salt Lake City, UT, United States; Eric W. Glissmeyer, University of Utah School of Medicine, Salt Lake City, UT, United States

Sarah Becker, DO (she/her/hers)
Assistant Professor, Medical Director Acute Care Telehealth
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Bedside providers in pediatric emergency, hospitalist, and critical care medicine often serve as consultants to referring providers and accepting physicians for patient transfer. Dedicated pediatric telemedicine providers integrated in transfer care may decrease unnecessary transfers and keep patients closer to home via tele-consultation.
Objective: Describe the disposition outcomes of patients before and after addition of a dedicated pediatric telemedicine provider at a large integrated healthcare organization in the United States.
Design/Methods: A pediatric telemedicine program was launched February 5, 2024 in a large integrated hospital system. Eleven board-certified pediatric emergency medicine and ten board-certified pediatric ICU physicians participated as pediatric telemedicine providers stationed at a transfer center. Data from 2/5/2024-10/5/2024 with dedicated pediatric telemedicine provider involvement were compared to the same dates in 2023 when bedside providers had been involved. Transfers are defined as patients transported from referring hospitals to pediatric-specific units. Consults are defined as patients not being transferred after medical consultation was provided.
Results: In the first eight months since its inception, the designated pediatric telemedicine provider answered calls on 2464 of 5162 (48%) patients. This provider was staffed 36% of the time (5/7 days per week, 12-hr shifts).
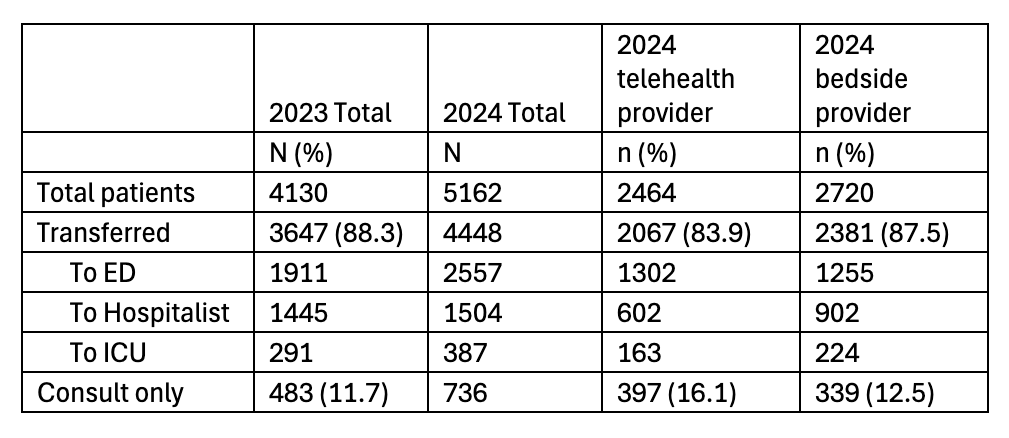
Table 1 describes dispositions of patients in 2023 (all calls managed by bedside providers) and 2024 (calls managed by pediatric telemedicine provider vs bedside providers). The proportion of transferred vs consults when managed by bedside providers were similar in 2023 vs 2024 (88.3 vs 87.5% and 11.7 vs 12.5%, p=0.34). In 2024, patients managed by the telemedicine provider, compared to calls taken by bedside providers, were transferred less often and more frequently managed as consults (83.9 vs 87.5% and 16.1 vs 12.5, p< 0.001).
Conclusion(s): The addition of a dedicated pediatric telemedicine provider decreased the number of pediatric patients transferred from referring facilities and increased patients managed by consultation. Further research is needed to explore clinical efficacy, and patient and referring provider satisfaction.
Table 1: Patient disposition before and after implementation of a pediatric telemedicine provider program