Neonatal Nephrology/AKI 1
Session: Neonatal Nephrology/AKI 1
001 - Acute Kidney Injury and Subsequent Risk of Late-Onset Infection among Extremely Low Gestational Age Newborns
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 1.4005
Megan J.. Turner, University of Colorado School of Medicine, Denver, CO, United States; Russell Griffin, University of Alabama at Birmingham, Birmingham, AL, United States; Meredith P. Schuh, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Keia R. Sanderson, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Cara Slagle, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; David Askenazi, University of alabama at birmingham, Birmingham, AL, United States; Katja Gist, Children's Hospital Medical Center (Cincinnati), Cincinnati, OH, United States; Shina Menon, Stanford University School of Medicine, Palo Alto, CA, United States
- MT
Megan J. Turner, MD, MPH (she/her/hers)
Neonatologist, Assistant Professor of Pediatrics
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Extremely low gestational age newborns (ELGAN) are at high risk for both acute kidney injury (AKI) and late-onset infection (LOI). AKI is a known risk factor for de novo sepsis and infection in critically ill children and adults. An association between AKI and subsequent LOI has not been demonstrated among ELGANs.
Objective: To determine whether an episode of acute kidney injury is associated with risk for subsequent late-onset infection among ELGANs.
Design/Methods: This was a secondary analysis of a multicenter, prospective study of ELGANs in the Preterm Erythropoietin for Neuroprotection Trial (PENUT) between December 2013-September 2016. Our analysis included infants who survived ≥7 days and had complete serum creatinine and urine output data. The primary outcome was any LOI, starting at least 72 hours after AKI. A time-varying Cox proportional hazards model was used to estimate adjusted hazard ratios of antecedent AKI and LOI.
Results: 872 infants were included. 332/872 (38%) experienced AKI. 552/872 (63%) experienced any LOI. 336/872 (38.5%) of late-onset infections were culture-positive, and 216/872 (24.8%) were culture-negative. After adjusting for gestational age, sex, postnatal steroid use, vancomycin or gentamicin receipt for ≥72 hours, birthweight, and 5-minute APGAR score, any AKI was associated with increased hazard of subsequent LOI (adjusted HR (aHR): 1.47; 95% CI: 1.15-1.87). When stratified by length of time between AKI and infection, the strongest hazard ratio was seen for culture-positive infection occurring at or beyond 21 days after the AKI event (aHR 2.48, 95% CI 1.56-3.96).
Conclusion(s): In this secondary analysis of PENUT trial participants, AKI was associated with an increased hazard of subsequent LOI in a large cohort of ELGANs. Identifying infants at highest risk for AKI could mitigate subsequent infectious complications in this high-risk population.
Figure 1. Patient Flow Diagram
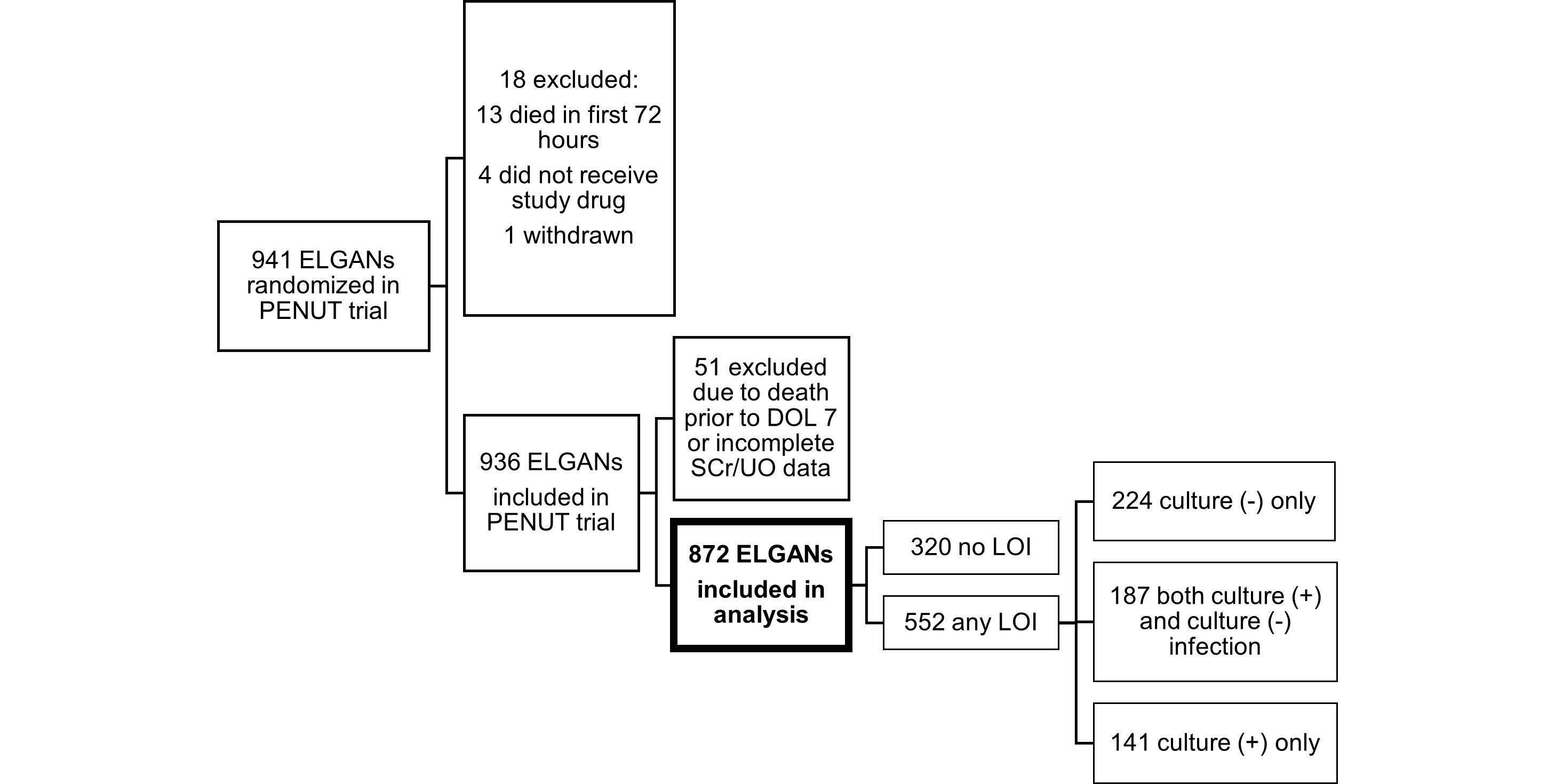
Table 1. Demographic and clinical factors compared by infection status (n=872)
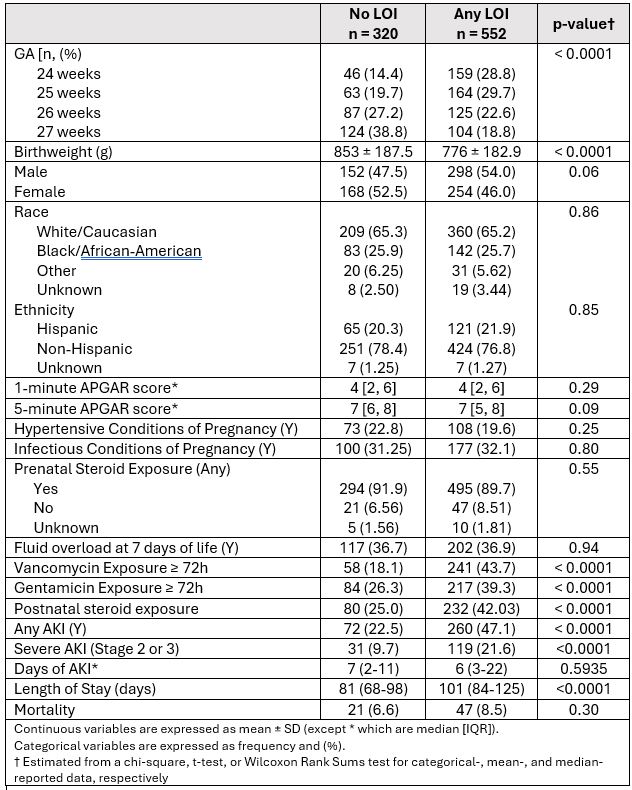
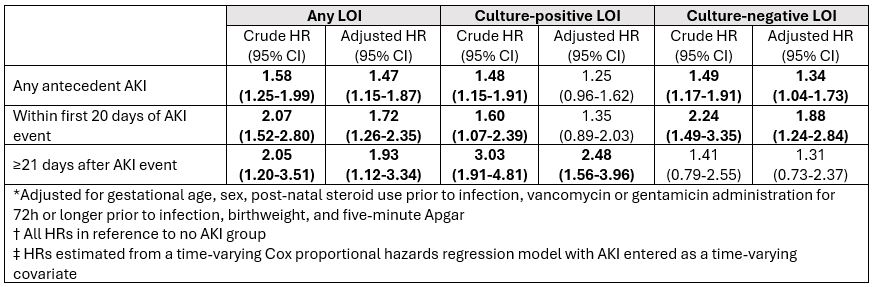
Table 3. Crude and adjusted* hazard ratios (HRs) and associated 95% confidence intervals (CIs) for the association between acute kidney injury (AKI) and late-onset infection by the timing of antecedent AKI.