Back
Background: The surge of anti-transgender legislation across the United States poses a significant threat to the availability of gender-affirming care for transgender and gender-diverse (TGD) adolescents. This study explores the ethical challenges faced by Adolescent Gender-Affirming Providers (AGAPs) navigating their professional obligations amidst these restrictive laws. The analysis is framed by key bioethical principles: autonomy, justice, beneficence, and non-maleficence.
Objective: This study aimed to understand the ethical implications of anti-transgender legislation on AGAPs and explore their perspectives on related bioethical dilemmas.
Design/Methods: In-depth interviews were conducted with 32 Adolescent Gender-Affirming Providers in states with active or proposed bans on adolescent gender-affirming care between March and July 2022. Participants were recruited via professional listservs and snowball sampling, ensuring representation from the South and Midwest regions, which are regions most impacted by legislative circumscription. Thematic analysis was performed with both inductive and deductive coding, using MAXQDA software. The study prioritized participant anonymity, and a diverse research team—including members from the queer and trans communities—ensured nuanced interpretation. This study was deemed exempt by the IRB, and informed consent was obtained.
Results: Participants described facing profound ethical dilemmas stemming from anti-transgender legislation. They reported balancing their ethical duty to “do no harm” with the risk of legal repercussions for providing necessary care. The primary themes included anticipatory anxiety, professional risk, ethical conflict, and moral distress, which impacted their capacity to deliver comprehensive and compassionate care to TGD youth. Among the 32 participants, 50% (n=16) were physicians (MD/DO), 19% (n=6) were clinical psychologists, 16% (n=5) were counselors or therapists, 6% (n=2) were nurse practitioners, and one was a chaplain.
Conclusion(s): Anti-transgender legislation exacerbates the ethical challenges faced by Adolescent Gender-Affirming Providers, undermining the principles of medical ethics and the right of TGD youth to access care. These restrictions contribute to increased stress and ethical conflict for providers, threatening the quality of care for TGD adolescents. Findings emphasize the need for policies that respect both the autonomy of TGD individuals and the ethical imperatives of healthcare providers, advocating for legislation that aligns with core healthcare ethics.
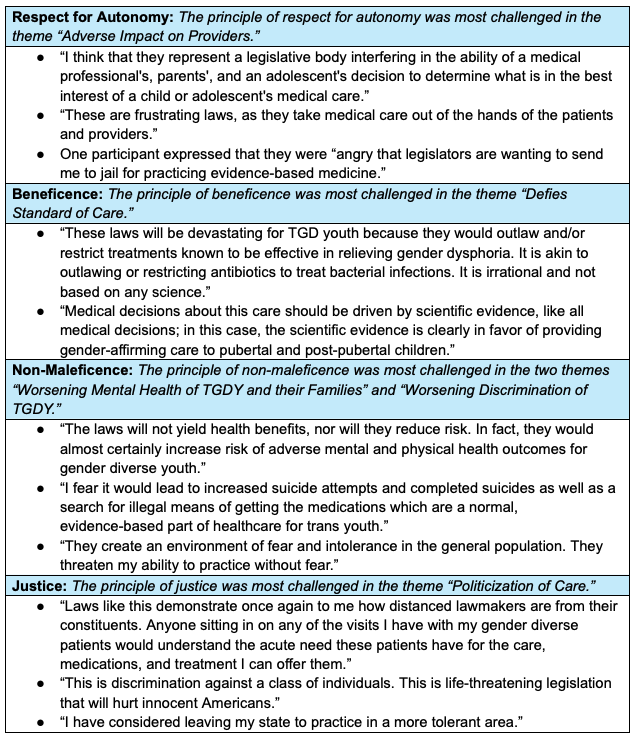
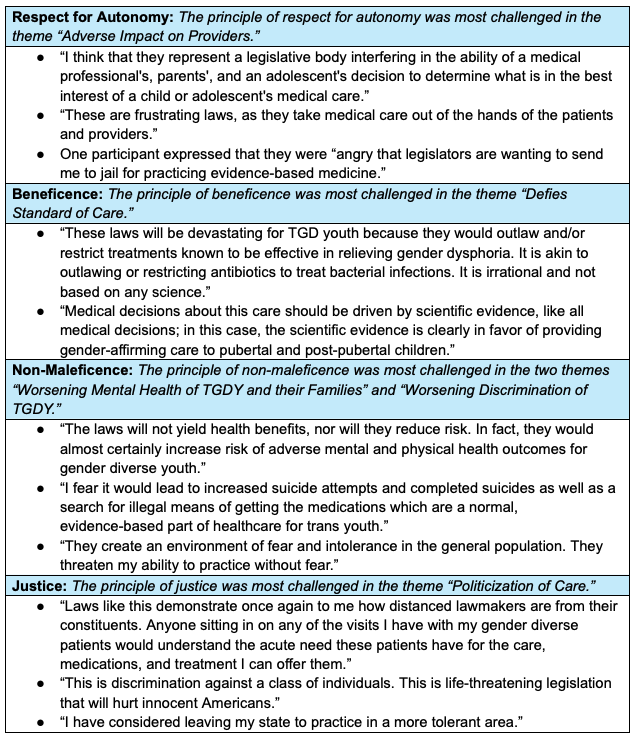
Table 1: Representative Quotes
Clinical Bioethics
Session: Clinical Bioethics
574 - Between Oath and Legislation: Navigating Bioethical Dilemmas in Gender-Affirming Care Amidst Anti-Transgender Legislation
Saturday, April 26, 2025
2:30pm – 4:45pm HST
Ari Gzesh, University of Pennsylvania, Philadelphia, PA, United States; Scott K. Jelinek, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Emily Rider-Longmaid, Children’s Hospital of Philadelphia, Philadelphia, PA, United States; Kristine Gamarel, University of Michigan, Ann Arbor, MI, United States; Jaclyn MW. Hughto, Brown University School of Public Health, Boston, MA, United States; Kacie Kidd, West Virginia University School of Medicine, Morgantown, WV, United States; Brittany Charlton, Harvard Medical School, Boston, MA, United States; Landon Hughes, Harvard Medical School, Boston, MA, United States

Ari Gzesh, MSW (they/them/theirs)
PhD Candidate
University of Pennsylvania
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The surge of anti-transgender legislation across the United States poses a significant threat to the availability of gender-affirming care for transgender and gender-diverse (TGD) adolescents. This study explores the ethical challenges faced by Adolescent Gender-Affirming Providers (AGAPs) navigating their professional obligations amidst these restrictive laws. The analysis is framed by key bioethical principles: autonomy, justice, beneficence, and non-maleficence.
Objective: This study aimed to understand the ethical implications of anti-transgender legislation on AGAPs and explore their perspectives on related bioethical dilemmas.
Design/Methods: In-depth interviews were conducted with 32 Adolescent Gender-Affirming Providers in states with active or proposed bans on adolescent gender-affirming care between March and July 2022. Participants were recruited via professional listservs and snowball sampling, ensuring representation from the South and Midwest regions, which are regions most impacted by legislative circumscription. Thematic analysis was performed with both inductive and deductive coding, using MAXQDA software. The study prioritized participant anonymity, and a diverse research team—including members from the queer and trans communities—ensured nuanced interpretation. This study was deemed exempt by the IRB, and informed consent was obtained.
Results: Participants described facing profound ethical dilemmas stemming from anti-transgender legislation. They reported balancing their ethical duty to “do no harm” with the risk of legal repercussions for providing necessary care. The primary themes included anticipatory anxiety, professional risk, ethical conflict, and moral distress, which impacted their capacity to deliver comprehensive and compassionate care to TGD youth. Among the 32 participants, 50% (n=16) were physicians (MD/DO), 19% (n=6) were clinical psychologists, 16% (n=5) were counselors or therapists, 6% (n=2) were nurse practitioners, and one was a chaplain.
Conclusion(s): Anti-transgender legislation exacerbates the ethical challenges faced by Adolescent Gender-Affirming Providers, undermining the principles of medical ethics and the right of TGD youth to access care. These restrictions contribute to increased stress and ethical conflict for providers, threatening the quality of care for TGD adolescents. Findings emphasize the need for policies that respect both the autonomy of TGD individuals and the ethical imperatives of healthcare providers, advocating for legislation that aligns with core healthcare ethics.
Table 1: Representative Quotes