Mental Health 2
Session: Mental Health 2
765 - Analysis of Perinatal Mood and Anxiety Disorders (PMADs) Resources Provided in High-risk Pediatric Areas
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 765.3939
John C. Pruett, Children's National Hospital, Washington, DC, United States; Sofia I. Perazzo, Childrens National Hospital, North Bethesda, MD, United States; Thevaa Chandereng, Childrens National Hospital, Silver spring, MD, United States; Lamia Soghier, George Washington University School of Medicine and Health Sciences, Washington, DC, United States; Lenore Jarvis, Children's National Hospital, Washington, DC, United States

John C. Pruett, MD (he/him/his)
PGY3 - Pediatric Resident Physician
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Perinatal mood and anxiety disorders (PMADs) have a known prevalence of 10-15% in outpatient settings; with high rates of positive screens in the pediatric emergency department (PED) (16%-27%) and neonatal intensive care units (NICUs) (24%-44%). Given this, our PED and NICU screen for PMADs and provide resources to caregivers, as needed.
Objective: To describe the types of resources given to caregivers who screen positive for PMADs in the PED and NICU, determine frequencies and association of resources provided by race and ethnicity, and the patient’s Distressed Community Index (DCI) Score.
Design/Methods: Data on type of resources and number of visits was collected from September 2022 to November 2023 in the PED and the NICU. All caregivers of patients under 7 months presenting to the PED and all caregivers of NICU infants were eligible. Resources were offered to families with positive screens. Data on resources offered was collected and grouped into five categories. Information on patient race, ethnicity and ZIP Code were obtained from the electronic medical record. The ZIP Code was used to calculate the patient’s Distressed Community Index (DCI) Score. Frequencies were calculated using descriptive statistics and odds ratio (OR) was calculated using univariable analysis.
Results: 153 caregivers (113 PED, 34 NICU, 6 other; majority mothers (85%) and non-Hispanic Black (42%); Table 1) were included. 93% of families received social support services, 28% financial support services, 71% ancillary support services, and 43% were referred to a medical provider. Notably, 26/65 (40%) of non-Hispanic Black families were provided financial support versus 1/19 (5%) of non-Hispanic White families (p=0.009). There were no statistically significant differences in resource utilization amongst DCI levels (Table 1 and 2). There was a statistically significant difference between frequency of referral to medical providers, ancillary services, and education between PED and NICU (Table 1 and 2).
Conclusion(s): Amongst caregivers who screened positive for PMADs, the most common resources provided were social support and ancillary services, reflecting a need for social workers and resources, regardless of family socioeconomic status. Elucidating an improved understanding of what types of resources caregivers need; healthcare systems can better grow to serve infants and their families.
Table 1. PMAD Positive Screen Resource Referral Characteristics (N= 153)
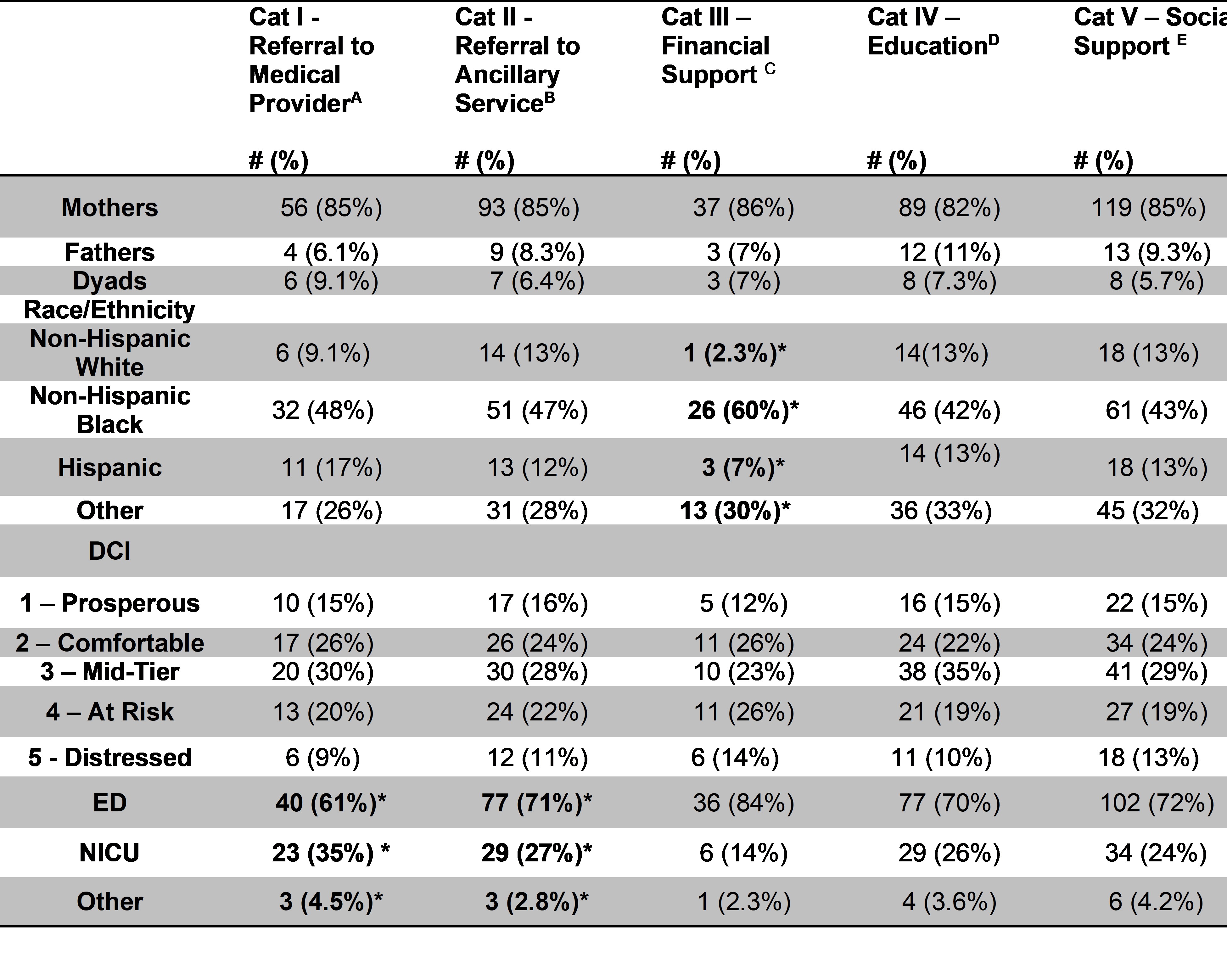 *p < 0.05
*p < 0.05A-Includes communication with primary team, psychiatry, community health, or substance use physicians
B-Includes case management, psychology, child protective services, lactation, chaplaincy services, therapist, child life specialist
C-newborn supplies, WIC referral, assistance with insurance, financial assistance
D-newborn education, facilitating treatment adherence, motivational interviewing
E-patient advocacy, grief counseling, crisis intervention, custody arrangements, referral to support group
Table 2. Factors Associated with Positive PMAD Screen Resource Allocation (N= 153)
.jpg) *p < 0.05
*p < 0.05** Sample size not sufficient for calculation

