Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
076 - Anticoagulation Practices for Neonatal Respiratory ECMO Therapy within the Children’s Hospitals Neonatal Consortium
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 76.3700
Sandy Johng, Seattle Children's Hospital, Seattle, WA, United States; Natalie Rintoul, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Mihai Puia-Dumitrescu, University of Washington School of Medicine, Seattle, WA, United States; Sarah Handley, University of Washington School of Medicine, Seattle, WA, United States; Zeenia Billimoria, University of Washington School of Medicine, Seattle, WA, United States; Katrin Lichtsinn, Seattle Children's, Seattle, WA, United States; Larissa A.. Yalon, Seattle Children's Hospital, Seattle, WA, United States; James Connelly, Children’s Hospital of Philadelphia, Philadelphia, PA, United States; Nicholas Carr, Intermountain Health, Sandy, UT, United States; Carly Heyrend, Primary Children's Hospital, Salt Lake City, UT, United States; Franscesca Miquel-Verges, University of Arkansas for Medical Sciences, Little Rock, AR, United States; David McCulley, University of California, San Diego School of Medicine, San Diego, CA, United States; Michelle Yang, University of Utah School of Medicine, Salt Lake City, UT, United States; Leslie Lusk, Benioff Children's Hospital Oakland, Oakland, CA, United States; Sharada H. Gowda, Baylor College of Medicine, Houston, TX, United States; Kelsey A.. Montgomery, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Robert DiGeronimo, Seattle Children's, Seattle, WA, United States

Sandy Johng, MD (she/her/hers)
Assistant Professor of Pediatrics
Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Bleeding and thrombotic events are the leading cause of morbidity and mortality associated with neonatal extracorporeal membrane oxygenation (ECMO) as reported in the ELSO registry. There is insufficient high-quality evidence for anticoagulation management, leading to wide practice variation between centers.
Objective: Our objective was to describe anticoagulation practices for neonatal respiratory ECMO therapy within the Children’s Hospitals Neonatal Consortium (CHNC).
Design/Methods: We developed an ECMO anticoagulation survey that underwent pretesting and pilot testing from multi-center experts in the field. The survey was distributed via RedCap to members of the CHNC ECMO Focus Group from April to May 2024. For centers with multiple responses, data was combined to a single response per center. Results were summarized via counts and proportions.
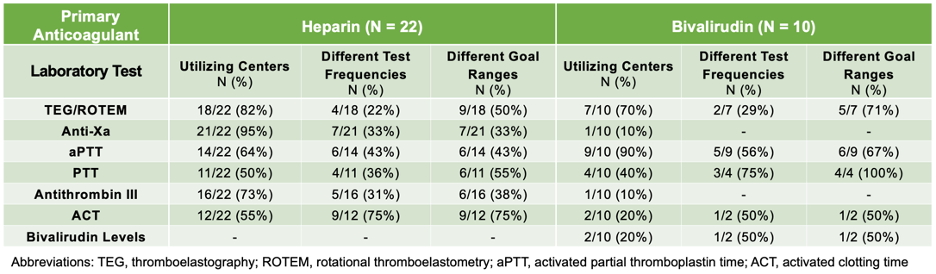
Results: We received 39 responses from 32/37 (86%) centers. 14/32 (44%) were from high-volume centers with greater than 10 neonatal respiratory ECMO cases per year. Type of circuit equipment varied widely between centers regarding pump type, system, and oxygenator (Figure 1). Bivalirudin was the primary anticoagulant in 10/32 (31%) centers, with the remainder (22/32, 69%) using heparin (Figure 2). Among centers using heparin first-line, 15/22 (68%) used bivalirudin second-line for a variety of indications (Figure 2A). The types, frequency, and target ranges of coagulation laboratory tests to monitor anticoagulation effectiveness varied between centers (Table 1).
Conclusion(s): There is considerable heterogeneity in anticoagulation management for neonatal respiratory ECMO within the CHNC. Variation in circuit components and build makes comparison of diverse anticoagulation practices difficult. There is a need for high-volume centers to standardize circuit components, build, and anticoagulation management to investigate how to prevent bleeding and clotting complications in neonatal patients receiving ECMO therapy.
Figure 1: Comparative chart of circuit components and primary anticoagulant by CHNC center.
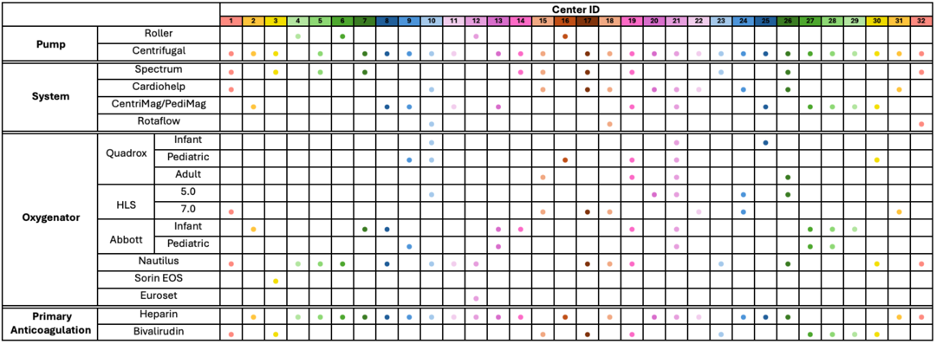
Figure 2: Primary anticoagulant. Figure 2A: Use of bivalirudin as second-line anticoagulant at centers using heparin first-line
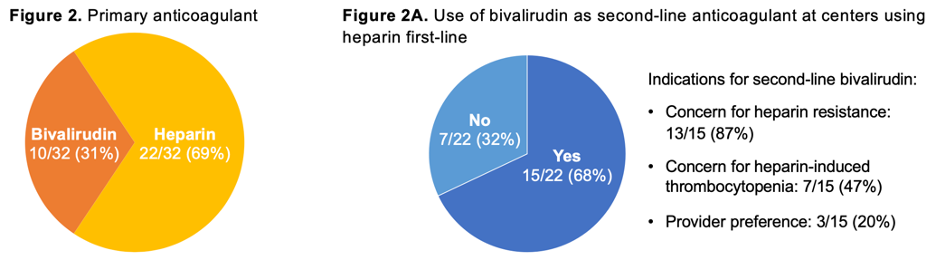
Table 1: Coagulation laboratory test utilization among heparin versus bivalirudin primary anticoagulant centers.