Hospital Medicine 2: Quality Improvement
Session: Hospital Medicine 2: Quality Improvement
567 - Reducing Overnight Vital Signs Checks: A quality improvement project to decrease sleep disturbances on the inpatient pediatric unit with sleep-friendly vitals
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 567.6402
Monica Saw-Aung, Jacobi Medical Center, Bronx, NY, United States; Nawal Saeed, Jacobi Medical Center Albert Einstein College of Medicine, Bronx, NY, United States; Raidour Ahmed, Jacobi Medical Center, Bronx, NY, United States
Monica Saw-Aung, MD (she/her/hers)
Resident Physician
Jacobi Medical Center
Bronx, New York, United States
Presenting Author(s)
Background: Sleep quality is often overlooked in hospitalized pediatric patients. Nighttime vital checks are typically performed per protocol rather than medical necessity. This project aims to enhance the use of sleep-friendly vital orders for eligible patients to reduce inpatient sleep disturbances.
Objective: The objective is to increase the usage of sleep-friendly vitals (SFV) placed for eligible patients on the inpatient pediatric unit in our inner-city community hospital by 25% over 12 months.
Design/Methods: A survey was completed by patients or their caretakers to name the sources of overnight sleep disruptions. Vital sign checks were the leading cause of inpatient sleep disruptions (28%). As baseline data, the usage of SFV orders in clinically stable patients between January and March 2024 was 47.5%. SFV-eligible patients were defined by the following criteria: age >30 days, normal vital signs in the previous 24 hours, no surgeries in the previous 24 hours, and no medications that can affect vital signs (opioids, albuterol, magnesium, antihypertensives). The primary target patients were those medically cleared but on social holds, awaiting durable medical equipment or inpatient psych placement. The main intervention, initiated in early April 2024, was the integration of SFV status into morning rounds, resident handoffs, and nursing huddles. SFV were discussed and ordered for eligible patients. The outcome measure was the percentage of eligible patients with a SFV order. A balancing measure was tracking the number of PICU transfers among patients with a SFV order.
Results: On average, the percentage of eligible patients with SFV orders placed increased from 47.50% in the pre-intervention period (January to March 2024) to a monthly average of 61.17% (April to September 2024), an increase of 13.67% with 0 PICU transfers among these patients.
Conclusion(s): Following an intervention that integrated SFV into the workflow, the average percentage of SFV orders for eligible patients rose by 13.67%, which fell short of our 25% target. This outcome suggests the need for further analysis and implementing more measures to increase the use of SFV in clinically stable patients on the pediatric floor.
Potential Hospital Sleep Disruptions and Noises Questionnaire
.png) A survey was completed by patients or their caretakers to name the sources of overnight sleep disruptions and rank their intrusiveness on a Likert scale of 1 to 5. Vital sign checks were the leading cause of inpatient sleep disruptions (28%).
A survey was completed by patients or their caretakers to name the sources of overnight sleep disruptions and rank their intrusiveness on a Likert scale of 1 to 5. Vital sign checks were the leading cause of inpatient sleep disruptions (28%).SFV orders placed on eligible patients discharged from January to September 2024
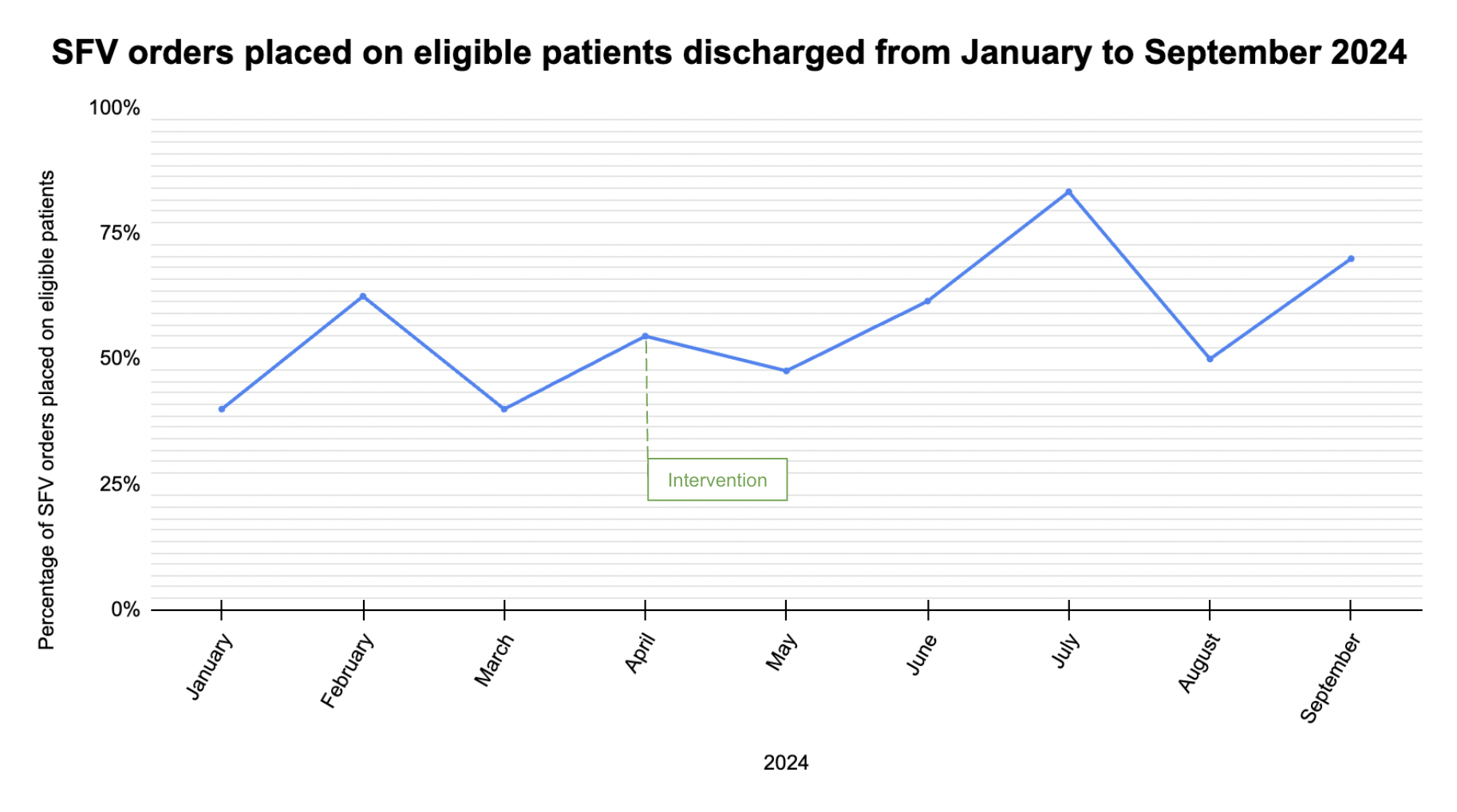 The percentage of SFV orders placed on eligible patients discharged from the inpatient pediatric unit were tracked on a monthly basis from January 1, 2024 to September 30, 2024. An intervention integrating SFV status into morning rounds, resident handoffs, and nursing huddles was initiated at the beginning of April.
The percentage of SFV orders placed on eligible patients discharged from the inpatient pediatric unit were tracked on a monthly basis from January 1, 2024 to September 30, 2024. An intervention integrating SFV status into morning rounds, resident handoffs, and nursing huddles was initiated at the beginning of April. 

