Hypertension
Session: Hypertension
035 - Association of MASLD by ICD-10 CODES with Blood Pressure Severity, Target Organ Injury, and Cardiovascular Health: A SUPERHERO Analysis
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 35.3815
Maggie Murphy, University of Kentucky College of Medicine, Lexington, KY, United States; Andrew M. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Stefan G. Kiessling, Kentucky Children's Hospital, Lexington, KY, United States; Sahar Siddiqui, Texas Children's Hospital, Houston, TX, United States; Michael J. Walsh, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Elizabeth A. Onugha, Baylor College of Medicine, Houston, TX, United States

Margaret Murphy, PhD, RD (she/her/hers)
Assistant Professor/Pediatric Renal Dietitian
University of Kentucky College of Medicine
University of Kentucky Healthcare
Lexington, Kentucky, United States
Presenting Author(s)
Background: Metabolic dysfunction-associated steatotic liver disease (MASLD) has become the most common chronic liver disease worldwide with prevalence increasing in youth with obesity. Patients with MASLD often present with several comorbidities including hypertension (HTN) however, it is unknown if youth with MASLD and HTN have worse cardiovascular health.
Objective: Investigate the relationships among pediatric MASLD and BP severity, target organ injury (TOI), and cardiovascular health at baseline in youth with HTN disorders.
Design/Methods: Cross sectional analysis of baseline data from the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a multisite retrospective cohort of youth referred to subspecialty care for hypertension disorders using electronic health record data. Inclusion criteria were an initial subspecialty clinic visit for HTN disorders identified by ICD-10 codes from 1/1/2016–12/31/2023 and age < 19 years. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 codes. Exposure included MASLD identified by ICD-10 codes. Unadjusted generalized linear models estimated the association of MASLD with the outcomes of BP severity with z-scores and classification per US guidelines, obesity by BMI or weight-for-length percentiles, TOI, dyslipidemia, hyperglycemia, LBW, and SGA by ICD-10 codes.
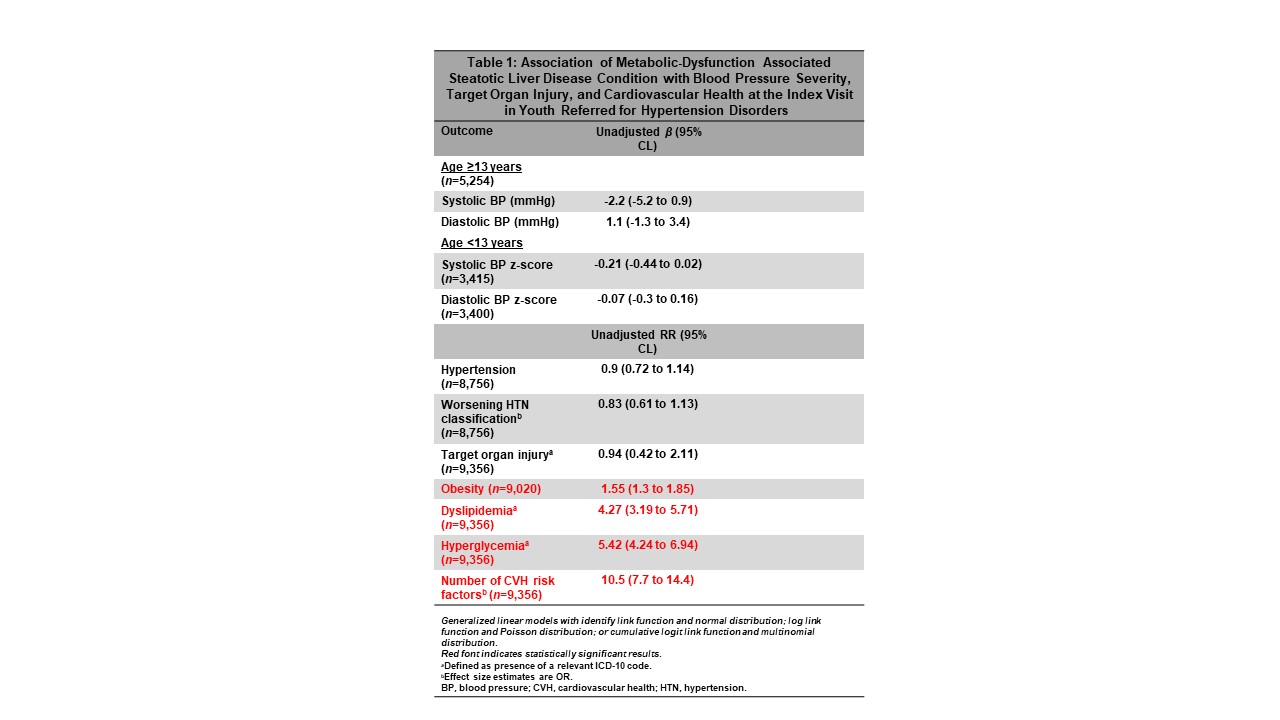
Results: Of the 9,356 participants, mean age was 12.8 ± 4.5, 62% were male, and 1% (n=132) had MASLD. Adolescents with MASLD had 2.2 mmHg lower SBP but 1.1 mmHg higher DBP. Participants with MASLD have a higher risk for obesity (RR 1.55, 95% CL 1.3–1.85), dyslipidemia (RR 4.27, CL 3.19–5.71), and hyperglycemia (RR 5.42, CL 4.24–6.94) but less risk for BP severity and TOI (RR 0.94, CL 0.42– 2.11).
Conclusion(s): In a large multisite cohort of youth referred for HTN disorders, MASLD is associated with heightened risk for several cardiovascular health risk factors. Our data suggest an increased prevalence for MASLD in youth with HTN disorders. Future studies will investigate causes of health care disparities to inform future management of youth with HTN disorders and other comorbidities including MASLD.
Association of Metabolic-Dysfunction Associated Steatotic Liver Disease Condition with Blood Pressure Severity, Target Organ Injury, and Cardiovascular Health at the Index Visit in Youth Referred for Hypertension Disorders