Quality Improvement/Patient Safety 5
Session: Quality Improvement/Patient Safety 5
469 - “Implementation Design Thinking” as a Guide to Rolling Out a New Digital Health Curriculum in the Emergency Department for Youth with Suicidality
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 469.3807
Mary Arakelyan, Children's Hospital at Dartmouth-Hitchcock, Lebanon, NH, United States; Stephanie Doupnik, Vanderbilt University School of Medicine, Nashville, TN, United States; Christian D.. Pulcini, The University of Vermont Children's Hospital, Shelburne, VT, United States; Stephanie C. Acquilano, Geisel School of Medicine at Dartmouth, Lebanon, NH, United States; Abigail Palaza, Robert Larner, M.D., College of Medicine at the University of Vermont, Colchester, VT, United States; Polina Krass, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Diana Worsley, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Joel A. Fein, Children's Hospital of Philadelphia at the Perelman School of Medicine, University of Pennsylvania, Media, PA, United States; Kevin W. Pettijohn, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Jessica J. Albert, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jennifer L. Hughes, Nationwide Children's Hospital, Columbus, OH, OH, United States; JoAnna Leyenaar, Dartmouth Health Children's, Lebanon, NH, United States

Mary Arakelyan, MPH (she/her/hers)
Research Project Manager
Children's Hospital at Dartmouth-Hitchcock
Lebanon, New Hampshire, United States
Presenting Author(s)
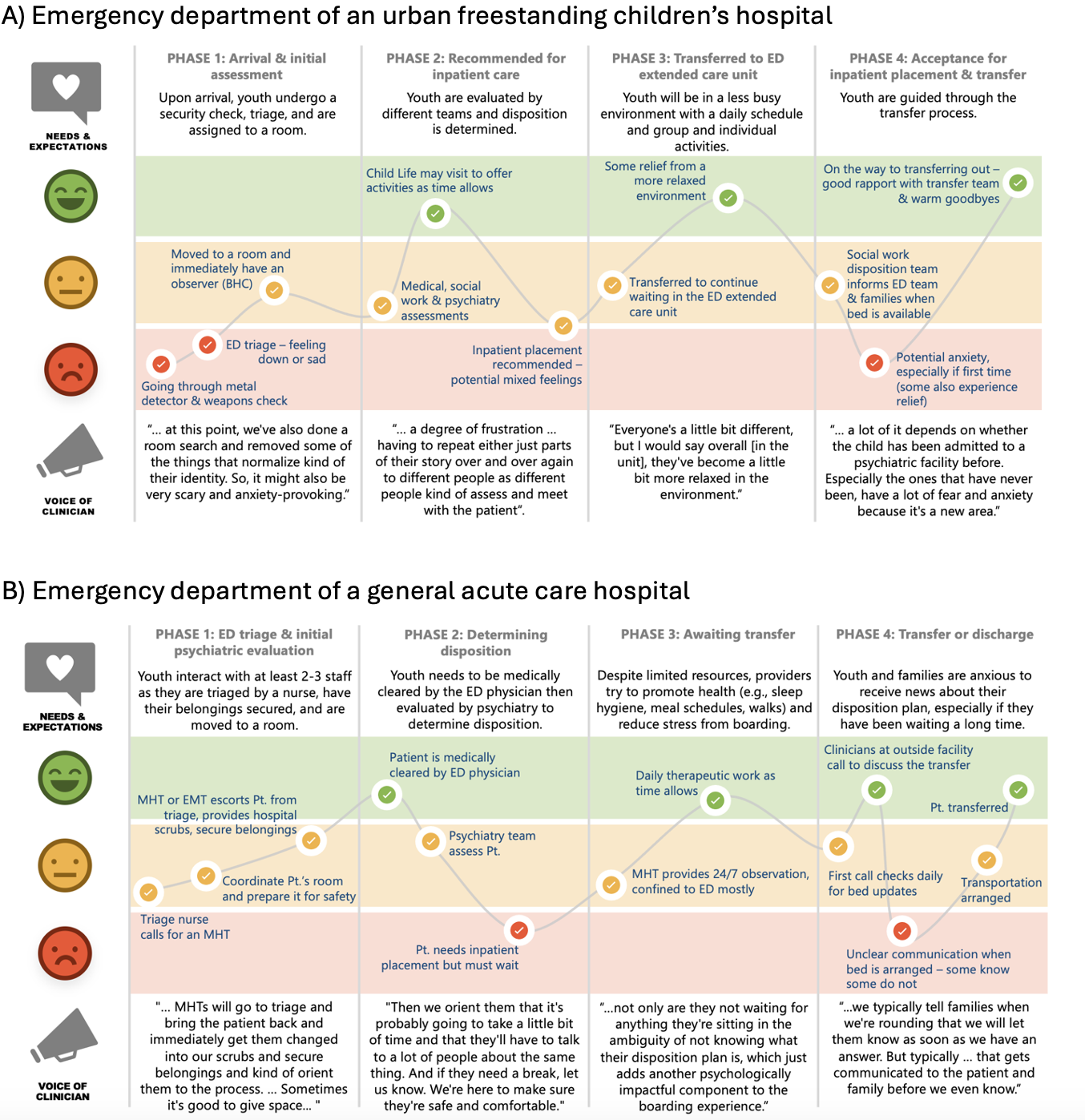
Background: Design thinking is a human-centered approach to problem-solving, widely used in product development industries. Its 5 stages – empathize, define, ideate, prototype and test – are applied iteratively with a focus on addressing user needs. Recognizing the potential of human-centered design to guide implementation of new clinical programs, research, and quality improvement efforts, we adapted the 5 stages of design thinking for this purpose, calling this adaptation “Implementation Design Thinking” (IDT, Table 1).
Objective: To apply IDT to guide implementation and pilot evaluation of a new digital health curriculum called I-CARE (“Improving Care, Accelerating Recovery & Education) for youth experiencing psychiatric boarding in 2 structurally diverse emergency departments (EDs).
Design/Methods: At each ED, we convened multidisciplinary leadership groups to support I-CARE implementation and engaged these groups in discussions and activities related to each IDT step. Discussions were audio recorded and analyzed thematically. We subsequently conducted a pilot study to evaluate I-CARE feasibility, using mixed methods to ascertain the experiences of youth 12-17 boarding due to suicidal ideation or attempt. Feasibility was defined as a Feasibility Implementation Measure score of >3 on the 5-point scale. Semi-structured interviews of youth participants were recorded, professionally transcribed, and analyzed thematically.
Results: Six IDT activity and discussion sessions with 22 clinician participants included 6 ED physicians, 4 psychiatrists, 3 nurses, and 9 social or behavioral health professionals. To empathize with youth experiencing boarding and chart the process at each ED, participants collaboratively developed journey maps (Figure 1). The ideation stage involved identification of local barriers and facilitators of program implementation. A storyboard was used to prototype the implementation process and iteratively revised (Figure 2). I-CARE was then tested with 25 youths; of 21 with a complete pre-discharge survey, n=20 (95%) rated I-CARE as feasible. Youth perspectives on program feasibility include user-friendliness of I-CARE activities, instructional value of I-CARE videos, and perceived relevance of the content which increased the likelihood and ease of engagement.
Conclusion(s): IDT provided a structured approach to implement this new digital health curriculum in two structurally diverse EDs, centering the experiences and perspectives of patients and clinicians. I-CARE was rated positively by youth, providing valuable preliminary data to guide future research and implementation efforts.
Table 1. Stages of Design Thinking for Implementation
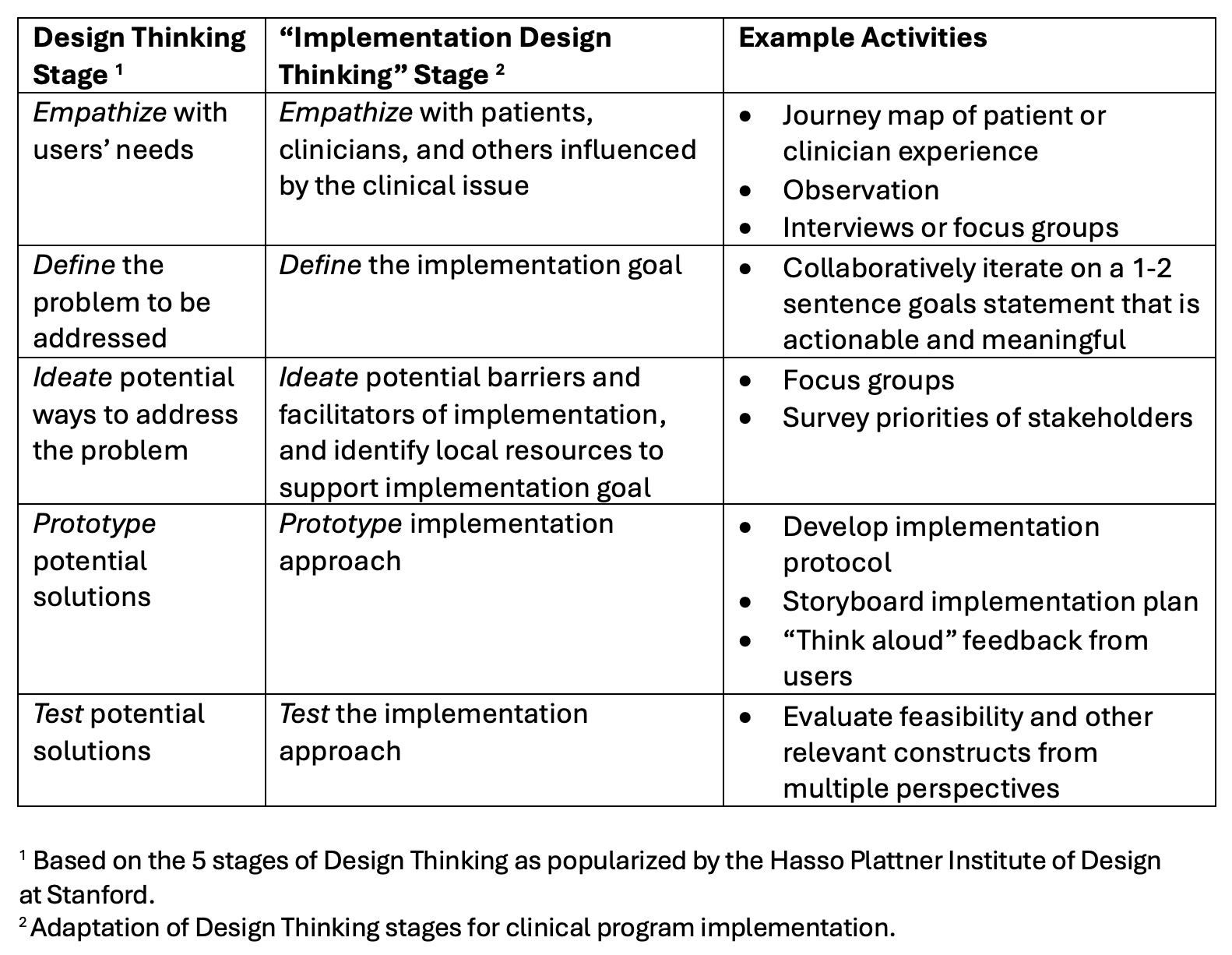
Figure 1. Journey Maps Depicting the Process and Emotional Experiences of Psychiatric Boarding at Two Implementation Sites
 Template for the journey maps was adapted from SlideModel.com: https://slidemodel.com/free-powerpoint-templates/free-customer-journey-map-template-for-powerpoint/.
Template for the journey maps was adapted from SlideModel.com: https://slidemodel.com/free-powerpoint-templates/free-customer-journey-map-template-for-powerpoint/. ED - emergency department; EMT - emergency medical technician; MHT - mental health technician; Pt. - patient.
Figure 2. A storyboard used to discuss the implementation plan with stakeholders and seek feedback on challenges at each step
.png)

