Medical Education 3: Simulation
Session: Medical Education 3: Simulation
200 - An interactive trauma training simulation curriculum to improve pediatric trainees’ level of comfort in trauma resuscitation skills
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 200.3823
Sofia Grigoria Athanasopoulou, Yale School of Medicine, New Haven, CT, United States; James Dodington, Yale University School of Medicine, NEW HAVEN, CT, United States; Isabel Gross, Yale School of Medicine, New Haven, CT, United States; Michael P.. Goldman, Yale School of Medicine, New Haven, CT, United States; Marc Auerbach, Yale School of Medicine, new haven, CT, United States

Sofia Grigoria Athanasopoulou, MD (she/her/hers)
Fellow in Pediatric Emergency Medicine
Yale School of Medicine
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Although pediatric trainees are often tasked with the management of traumatically injured patients, most training programs do not have a dedicated trauma training curriculum. To address this gap, we created and iteratively evaluated an open-access trauma simulation curriculum for pediatric trainees.
Objective: To use an interactive trauma training simulation curriculum to improve pediatric trainees’ level of comfort in trauma resuscitation skills.
Design/Methods: A curriculum was designed and implemented in a cohort of trainees in a pediatric residency program. The curriculum included a pre-learning video, a cognitive aid (image 1) and a 3-hour simulation session. Case-specific videos with patient animations and pre-recorded vital signs were designed and used to increase the fidelity of the simulations (image 2). Participants completed a 14-question retrospective pre-post survey. Descriptive statistics and paired t-tests were performed to analyze the data.
Results: A total of 50 trainees participated in 3 trauma simulation sessions, including 5 medical students, 11 interns, and 34 senior pediatric residents. Pre-simulation, 96% (48/50) trainees had participated in < 5 full trauma and 82% (41/50) in < 5 modified trauma activations in the ED. Roles in pediatric trauma care included: placing orders on the computer 64.58% (31/48) and family liaison 14.58% (7/48). Only 2.08% (1/48) of the trainees reported performing primary and secondary surveys. Using a 5-point Likert scale (0=extremely uncomfortable and 5=extremely comfortable), a statistically significant increase in participants’ level of comfort was observed in all the trauma resuscitations skills (table 1). There was a statistically significant increase in comfort levels performing a complete primary survey post-intervention (Mean = 4.02) compared to pre-intervention (Mean = 2.00), with a mean difference of 2.02 (p < 0.001), as well as a statistically significant increase in comfort performing a secondary survey post-intervention (Mean = 3.88) compared to pre-intervention (Mean = 2.06), with a mean difference of 1.82 (p < 0.001). After the simulation session 82% (41/50) of the trainees reported feeling more likely to participate in a trauma activation in the ED.
Conclusion(s): A trauma simulation curriculum was successful in increasing pediatric trainees’ level of comfort in key areas of pediatric trauma care. Future work can evaluate if improved confidence impacts practice and participation in trauma activations. Open-access simulation resources can help address the gap in trauma training for pediatric trainees.
Image 1. Cognitive aid
.png)
Image 2. Simulation video
.png)
Table 1. Assessment of Learners’ Comfort Levels in Pediatric Trauma Skills Before and After Simulations
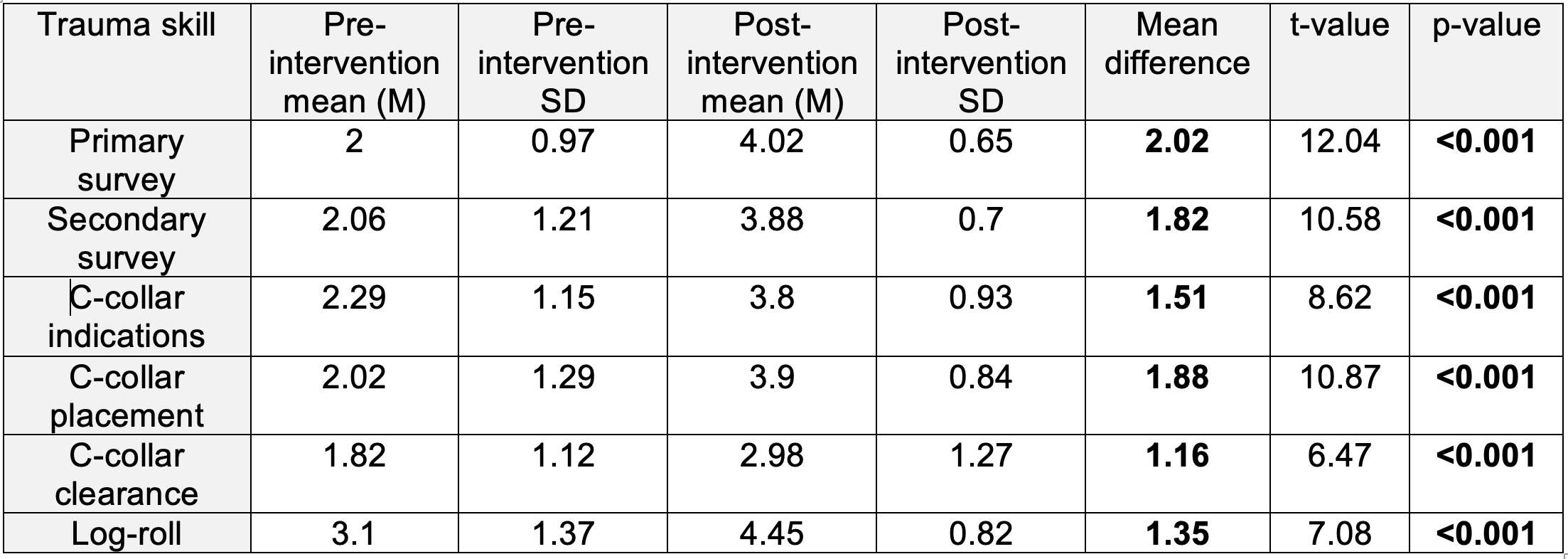 Range: 0 = Extremely Uncomfortable to 5 = Extremely Comfortable
Range: 0 = Extremely Uncomfortable to 5 = Extremely Comfortable
