Neonatal Hemodynamics and Cardiovascular Medicine 3
Session: Neonatal Hemodynamics and Cardiovascular Medicine 3
061 - 4D echocardiographic assessment of newborns with congenital heart disease during the transitional phase - a prospective study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 61.3826
Silvia Nogara, Università degli Studi di Verona, Vicenza, Veneto, Italy; Shiran S. Moore, Tel Aviv University, Port Washington, NY, United States; Daniela Villegas Martinez, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Adrian Dancea, MCH of MUHC, Montreal, PQ, Canada; Punnanee Wutthigate, Mahidol university, Bangkok, Krung Thep, Thailand; Jessica Simoneau, Montreal Children’s hospital, Vercheres, PQ, Canada; Marie Brossard-Racine, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Wadi Mawad, Mcgill university, Montreal, PQ, Canada; Tiscar Cavalle-Garrido, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Gianluca Bertolizio, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Gabriel Altit, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada
- SN
Silvia Nogara (she/her/hers)
Neonatologist
Università degli Studi di Verona
Vicenza, Veneto, Italy
Presenting Author(s)
Background: The hemodynamic transition to extra-uterine life in newborns with congenital heart defects (CHD) can be disrupted by the presence of shunts and the defect itself. Four-dimensional echocardiography (4D-ECHO) enables quantification of ventricular dimensions and performance. Understanding how the systemic ventricle adapts to these hemodynamic shifts may enhance patient management during this crucial period.
Objective: Investigate cardiac function and dimensions evolution during the first week of life in newborns with CHD using 4D-ECHO.
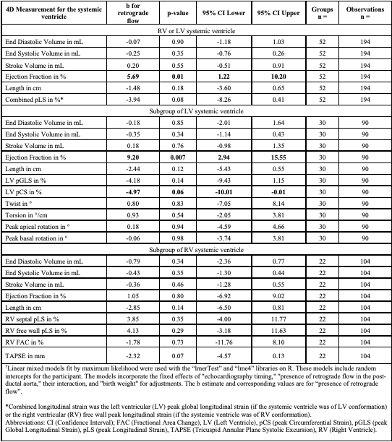
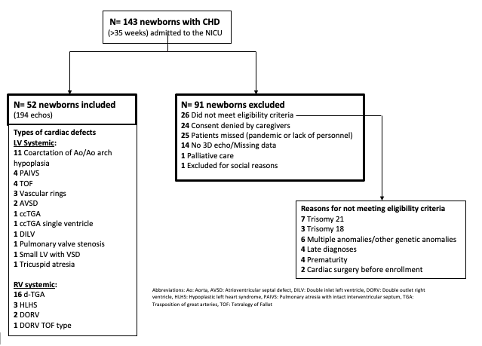
Design/Methods: Prospective, observational, single-center study including newborns with a diagnosis of congenital heart defects (CHD) admitted within their first week of post-natal life between 2019 and 2023. We included those born at ≥35 weeks prior to cardiac intervention. We excluded those with a genetic disorder or extracardiac anomalies. Daily 4D-ECHO were performed up to seven days of life (DOL) or until intervention/discharge. Images were analyzed offline by blinded evaluators. Systemic ventricular volumes and function were analyzed using linear mixed-effects models, adjusted for 4D-ECHO timing, birth weight, and diastolic retrograde flow in the descending aorta (dAo) at the echocardiography closest to DOL 7 (as a marker of systemic steal).
Results: Of the 143 newborns with CHD approached for eligibility during the study period, 52 (63% male, mean gestational age 38.5±1.3 weeks) met inclusion criteria, with 194 4D-ECHOs collected at various daily time-points (Figure 1). Forty percent of the cohort had a systemic right ventricle. Despite the hemodynamic burden associated with CHD, most 4D-ECHO parameters remained stable throughout the study. Right ventricular (RV) free wall peak longitudinal strain increased over time in those with a RV systemic ventricle (Figure 2). Patients with diastolic reverse flow in the descending aorta (dAo), all of whom had a large patent ductus arteriosus (PDA), exhibited higher ejection fraction (EF) in those with a LV systemic ventricle (Figure 3).
Conclusion(s): Systemic ventricular function in neonates with CHD remains largely stable during the first week of life, as assessed by 4D-ECHO. It remains unclear whether this stability represents a normal adaptation. Diastolic retrograde flow in the dAo was associated with an increased EF, as expected when the LV encounters low afterload due to decreasing pulmonary vascular resistance in the presence of a large PDA. Future studies are needed to investigate the relationship between these functional parameters and clinical outcomes.
Study flowchart
Linear mixed-effect model for 4D-ECHO parameters by “echocardiography timing”
.png)
Linear mixed-effect model for 4D-ECHO parameters by “presence of retrograde flow”